Zoo, we agree on so many things, I don't want it to seem that I'm stepping on your toes.
Not at all.

Posted 29 December 2006 - 11:42 PM
Zoo, we agree on so many things, I don't want it to seem that I'm stepping on your toes.
Posted 30 December 2006 - 12:06 AM
I say this not as a challenge to Christy's integrity...I've just heard of a condition called "meth mouth" -- so when I hear anyone claim to be a meth addict for multiple years (especially 10!), I find it hard to believe they could have their teeth in as good a shape as Christy's are in the video I linked to.
June 11, 2005
Grisly Effect of One Drug: 'Meth Mouth'
By MONICA DAVEY
From the moment on Thursday when the young man sat down in Dr. Richard Stein's dental chair in southwestern Kansas and opened his mouth, Dr. Stein was certain he recognized the enemy. This had to be the work, he concluded, of methamphetamine, a drug that is leaving its mark, especially in the rural regions of the Midwest and the South, on families, crime rates, economies, legislatures - and teeth.
Quite distinct from the oral damage done by other drugs, sugar and smoking, methamphetamine seems to be taking a unique, and horrific, toll inside its users' mouths. In short stretches of time, sometimes just months, a perfectly healthy set of teeth can turn a grayish-brown, twist and begin to fall out, and take on a peculiar texture less like that of hard enamel and more like that of a piece of ripened fruit.
The condition, known to some as meth mouth, has been studied little in dentistry's academic circles and is unknown to many dentists, whose patients are increasingly focused on cosmetic issues: the bleaching and perfect veneers of television's makeover shows. But other dentists, especially those in the open, empty swaths of land where methamphetamine is being manufactured in homemade laboratories, say they are seeing a growing number of such cases.
These are the same towns, in some cases, that have wrestled in recent years with shortages of dentists. They are places where dentists have struggled to sell their practices as populations shrink; where new dentists have been reluctant to settle, out of fear that they will not get enough business to make ends meet; and where political leaders have offered financial incentives to lure young dentists to town. For good or ill, meth mouth is creating more business.
East of Dr. Stein's Dodge City office, in Independence, Kan., Dr. Cynthia E. Sherwood said she too had seen such patients lately, including a woman whose teeth had been transformed into "little black stubs" too painful to brush and who wound up losing all her top teeth and six of her lower ones. Among similar patients Dr. Charles Tatlock has seen in his New Mexico office, he said, was one who, though only 17, needed dentures to replace his suddenly decayed teeth.
And in Tennessee, Dr. Daniel D. Roberts gave up his ordinary practice not long ago to handle a growing workload at 10 jails across the state, nearly a third of whose prisoners, he estimates, have ravaged teeth owing to methamphetamine.
"This is the worst thing to come along in a long time," Dr. Roberts said the other day. "At this point, I'm digging for roots. That's how I make my living."
Some dentists have their own hypotheses about precisely what causes the condition.
Dr. John W. Shaner, an associate professor at the Creighton University Medical Center School of Dentistry, in Omaha, said he believed that a combination of factors tied to the use of methamphetamine led to such enormous damage.
The drug itself, a synthetic stimulant that can be manufactured just about anywhere, causes dry mouth, Dr. Shaner said, and that in turn allows decay to start, since saliva is unavailable to help control bacteria in the mouth. The drug also tends to leave users thirsty and craving a constant supply of soda pop and other sugary drinks, which spur the decay; Mountain Dew, he said, has become the preferred drink of methamphetamine users. At the same time, the drug's highly addictive nature causes many users simply to stop doing what is needed to take care of themselves, including the brushing of teeth.
Other dentists said they suspected that the caustic ingredients of the drug - whether smoked, injected, snorted or eaten - contributed to the damage, which tends to start near the gums and wander to the edges of teeth. Among ingredients that can be used to make meth are red phosphorus found in the strips on boxes of matches and lithium from car batteries.
There are also dentists who point to methamphetamine users' tendency to grind and clench their teeth nervously, aggravating the frighteningly twisted and tangled look of meth mouth.
If the man sitting in Dr. Stein's Kansas office on Thursday, who readily admitted having used methamphetamine, gets all the work done that he needs - X-rays, fillings and crowns, and implants for the teeth now missing from his mouth - he will require many visits, and the bill could run to as much as $7,000.
Most dentists, though, say this is hardly the growth industry any of them would wish for. The patients are grim, their teeth grimmer. Many of these young people, the dentists say, may end up with no teeth at all but with dentures, which some in dentistry had come to believe would soon be mostly relics of the past, even for the elderly, in an age of water fluoridation and other technology.
"The real market for dentistry is in saving teeth, in helping people have dental health," said Dr. Stein, 57. "But I've seen a lot. I'm not a drug counselor, and I'm long past lecturing, but this is a sorry situation."
Dr. Shaner said meth mouth might be little recognized in many places - even as the drug has spread from one coast to the other and from rural areas into cities - because methamphetamine is a problem that has had a chance to sink in longer in places like Nebraska, Iowa and Missouri and because the effects to teeth are often most obvious in pockets like prison populations. He said he hoped to present information on the topic at a conference of the American Dental Association next year.
With the exception of a few formal studies, including one now beginning in New Mexico, meth mouth has so far been less a topic of academic analysis in the dental profession than a matter for casual phone conversations and e-mail exchanges between dentists in small places.
"The truth is, very little is known yet," said Dr. Stephen Wagner, who specializes in dentures and implants in his private practice and who in coming months will be studying 20 afflicted patients with Dr. Tatlock, an assistant professor at the University of New Mexico. "What I can tell you is what I have seen: It looks like someone has taken a hammer to these teeth and shattered them."
One of the strangest truths of the condition, dentists said, is that despite the truly grisly look, many patients do not report suffering from as much pain as one would expect. Or at least, these dentists said, they do not report such pain while still using methamphetamine.
Though the condition has begun turning up in private practices, particularly in cases of emergency care and among recovering addicts, it is far more prevalent in the dental offices of the nation's jails and prisons.
Local sheriffs in Midwestern and Southern counties have complained of soaring dental costs in their jails. In North Dakota, more dentures have been needed in the state penitentiary in the last few years, a development that officials attribute at least in part to methamphetamine. In North Carolina, dental workers in the Department of Correction learned about meth mouth during a training session this month; starting in July, new prisoners there will be screened for signs of dental problems connected to the drug.
In Minnesota's state corrections system, meanwhile, dentists' workloads are so full of gruesome methamphetamine-related matters that they are strained to get to other, less urgent cases: the routine cleanings and fillings of years past.
"All of our time is getting eaten up," said Dr. Stephen Boesch, a dentist who works at a Minnesota prison and who said he had begun to see the problem in a juvenile corrections center as well. "We're seeing this week in and week out."
Some dentists said they would never ask their patients about drug use; that is not their place, they said. Others said they would ask, but could not force the issue.
"That's the thing: you can't beat a confession from someone," said Dr. Eric Curtis, who shares a practice with his father in Safford, Ariz., and began seeing meth mouth four years ago.
"I suspect that many dentists are out there seeing this but don't know what they're seeing," said Dr. Curtis, a spokesman for the Academy of General Dentistry. "And most of them aren't going to know for sure."
The new business, he said, is actually a gloomy one for dentists in rural places like Safford.
"What dentists really make the money on is the happy stuff: the low-impact work with beautiful results," he said. "Nobody is happy when you pull a bunch of teeth and put in dentures."
Gretchen Ruethling contributed reporting for this article.
Posted 30 December 2006 - 05:21 AM
Posted 30 December 2006 - 11:02 PM
LOLIf you have a crack pipe in one hand and a 750mL bottle of half drunk Smirnoff in the other. That's not smart. There are better quality vodkas on the market!
Posted 31 December 2006 - 04:21 AM
The Meth-Mouth Myth
Our latest moral panic.
By Jack Shafer
Posted Tuesday, Aug. 9, 2005, at 6:34 PM ET
Moral panics rip through cultures, observed sociologist Stanley Cohen in 1972, whenever "experts" and the "right-thinking" folks in the press, government, and the clergy exaggerate the danger a group or thing poses to society.
Immigrants have been the subject of moral panics, as have alcohol, jazz, comic books, sex, street gangs, rock, video games, religious cults, white slavery, dance, and homosexuals. But in the United States, moral panics are most reliably directed at illicit drug users. No exaggeration or vilification directed their way is too outrageous for consideration.
For the last year, a moral panic about methamphetamine and its users has been gathering force, and last week it peaked as Slate's corporate sibling, Newsweek magazine, joined the crusade with a cover story. Calling methamphetamine "America's Most Dangerous Drug," the magazine also portrayed its use as "epidemic." In typical moral-panic fashion, Newsweek offered no data to anoint meth as the deadliest of drugs, nor did it prove its assertion that meth use is spreading like a prairie fire. Instead, the magazine relied almost exclusively on anecdotes from law enforcement officials, anti-drug politicians, and users (current and reformed) to stir up emotions against meth and meth-heads.
If you were to reduce the current moral panic to a single image, it would be a photo of a meth user whose gums are pus-streaked and whose rotting teeth—what teeth he still has—are blackened and broken. The affliction, tagged "meth mouth" in scores of articles, earns a prominent place in Newsweek's Grand Guignol coverage (see the picture in this Newsweek spread).
Although users have been snorting, smoking, injecting, and swallowing methamphetamine in great quantities for more than 40 years, the phrase meth mouth is brand new. It makes its first Nexis appearance in Investor's Business Daily as an unsourced one-liner in a Jan. 31, 2003, digest of news: "Methamphetamine's drying effect on saliva glands leads to tooth decay and gum disease, dentists say, a trend known as 'meth mouth.' "
More than two dozen different stories about meth mouth have appeared in Nexis since the IBD mention, but the majority of them fail to advance the story in any significant way. The better articles note, as IBD did correctly, that methamphetamine users suffer from dry mouth (xerostomia), which contributes to tooth decay and gum disease. Many of them also find that many users attempt to refresh their dry mouths with sugared sodas, which accelerates decay. The best articles explain that many meth-mouthers get that way because they've neglected brushing, flossing, and regular visits to the dentist. Such a regimen is almost always a prescription for tooth loss.
But most of the articles go off on tangents, blaming contaminants or the corrosive quality of meth itself. For instance, Minneapolis' Star Tribune (Jan. 6, 2005) writes that the "acidic nature of methamphetamine if it is smoked or snorted" plays a role (reprinted in shorter form). The St. Paul Pioneer Press (Jan. 6, 2005) finds that "acid in meth corrodes tooth enamel, letting decay-causing bacteria seep in."
The Kansas City Star (Jan. 26, 2005): "What causes the problems is the acid content in some of the ingredients used to make methamphetamine, including anhydrous ammonia, ether and lithium. The acid can decrease the strength of the enamel on the teeth." Nice try, Star, but anhydrous ammonia, ether, and lithium are not acids.
The AP (Feb. 2, 2005) points to contaminants as well: "Methamphetamine can be made with a horrid mix of substances, including over-the-counter cold medicine, fertilizer, battery acid and hydrogen peroxide"—chemicals that reduce saliva, which is needed to neutralize acids and clear food from the teeth. Later that same month, the AP (Feb. 21, 2005) says that "methamphetamine ingredients like hydrochloric acid and lye corrode teeth when users inhale the drug's smoke. The drug dries in users' mouths, drying saliva that would block the acid and letting food build up on the gums against the teeth."
The Albuquerque Journal (April 12, 2005) collects this artful anecdote from a local dentist: "Meth use is an emerging epidemic. ... It explodes people's teeth. It's like ice crystals forming in the crevices of rock, fracturing the teeth."
The New York Times (June 11, 2005) showcases the meth-mouth story on Page One: "Other dentists said they suspected that the caustic ingredients of the drug—whether smoked, injected, snorted or eaten—contributed to the damage, which tends to start near the gums and wander to the edges of teeth. Among ingredients that can be used to make meth are red phosphorus found in the strips on boxes of matches and lithium from car batteries."
The contaminant angle is complete misinformation. Dr. John R. Richards M.D., who studied tooth damage among 49 users in the late 1990s and co-wrote a paper on his finding for the August 2000 issue of the Journal of Periodontology, says users could consume pharmaceutical-grade methamphetamine and still lose their teeth.
The paper, titled "Patterns of Tooth Wear Associated With Methamphetamine Use," recorded the most dramatic tooth wear among methamphetamine users who preferred snorting meth over other means of administration. Frequent snorting of the drug inhibits blood flow to the arteries that service the top front teeth, the authors found, which weakens them. Also, most of study's subjects smoked tobacco, and the connection between smoking and bad teeth is well-known.
"Not all that much tooth damage could be caused in the short time methamphetamine is in your mouth," Richards says. He adds that upper teeth are more prone to drying than lower teeth. When meth users binge and pass out, they may sleep for a day or longer with their mouths open, further drying their uppers.
Richards calls neglect of basic hygiene the biggest cause of dental damage among users. "It's a lifestyle issue," he says.
None of the articles blaming "contaminated" methamphetamine for meth mouth cite any literature or authority, perhaps because it doesn't exist. Page 59 of this 1991 monograph from the U.S. National Institute on Drug Abuse surveys the scientific literature and finds examples of rare lead poisoning from bathtub meth (14 cases) but is silent on acids. Page 62 lists known organic contaminants in clandestinely made meth but concedes that no toxic reactions to the compounds have been reported.
The second press piece published on meth mouth should have served as a template for the reporters chasing the story. On April 5, 2004, the AP reported on meth mouth among inmates in North Dakota's state penitentiary. The peg for the story was that the prisoners were incurring gargantuan dental bills for you-know-what. From the AP story:
[Prison dentist Lonnie] Neuberger said he thinks there is a relationship between the chemicals in meth and tooth decay, but said there is little scientific evidence about the phenomenon.
Neuberger said malfunctioning salivary glands are another factor that causes tooth decay among meth users. The glands normally secrete saliva, which neutralizes acids present in the mouth and around teeth.
In meth users—partly because of the dehydration common because they do not drink enough fluids—salivary glands quit and swell shut.
The next sentence, also attributed to Neuberger, places the condition in a normalizing context:
The same thing often happens to the elderly because of inadequate hydration and side effects from medication. [Emphasis added.]
In other words, abstinent grandmothers and grandfathers, many of whom who couldn't spell methamphetamine if their lives depended on it, are sometimes victims of meth mouth!
The Merck Manual of Medical Information speaks articulately to the rampant tooth decay that follows salivary gland malfunction: "Because saliva offers considerable natural protection against tooth decay, an inadequate amount of saliva leads to more cavities—especially on the roots of teeth."
Many drugs—some of them in your medicine cabinet—inhibit saliva production. An AP story from October 1997, years before the meth moral panic set in, reports:
Hundreds of medicines that Americans take every day, from the country's most popular blood pressure pills to chewable vitamin C tablets, can cause serious tooth decay and gum disease, oral medicine experts told the American Dental Association.
One patient stuck his nitroglycerine tablets under his upper lip instead of under his tongue, where it was supposed to go. "And they ate a hole in his tooth," the AP writes. Nearly 20 percent of patients taking best-selling calcium channel blockers (Procardia, Cardizem, and Adalat) for high blood pressure and heart disease suffer gum swelling. Bacteria attack the inflammation, causing more swelling and serious gum disease ensues. Anti-epilepsy drugs, particularly Dilantin, and some amphetamines given to hyperactive kids cause similar swelling. Cyclosporin, which prevents organ rejection, can cause massive gum overgrowth.
The connections between drug abuse and tooth loss are established in the medical literature, even when the drug is booze. A recent study at the University of Buffalo found that alcohol abuse may lead to periodontal disease, tooth decay, and potentially precancerous mouth sores, but don't expect anybody to call it "Miller mouth."
Richards' paper has yet to be cited in a newspaper or magazine indexed by Nexis, perhaps because most reporters think of drug abuse in terms of criminal justice and moral panic. Had one journalist seriously considered covering meth mouth from a public health point of view, all he had to do is plug "methamphetamine and teeth" into PubMed, the free federal database, to find the Richards paper citation.
******
Give the New York Times an honorable mention for an April 12, 2005, story that discusses meth mouth from a public health point of view, stating that the poor dental and oral health of rural, ethnic, and disabled Americans has not improved since a surgeon general called attention to it in 2000 report. Thanks to the American Academy of Periodontology for providing the Richards article on short notice. Thanks to reader Jon Paul Henry for the moral-panic angle. Send e-mail containing an angle of your own to slate.pressbox@gmail.com. (E-mail may be quoted unless the writer stipulates otherwise.)
Jack Shafer is Slate's editor at large.
Article URL: http://www.slate.com/id/2124160/
Copyright 2006 Washingtonpost.Newsweek Interactive Co. LLC
Posted 06 January 2007 - 11:28 PM

Summary:
A new UCLA Neuroscience imaging study shows for the first time the selective pattern of destruction to the brain's memory, emotion and reward systems experienced by chronic methamphetamine users. Color, three-dimensional visualizations created from magnetic resonance images vividly show the damage. The study reveals the mechanism by which drug abuse damages the brain and suggests potential targets for therapy in recovering drug users. The research appears in the June 30 online edition of the peer-reviewed Journal of Neuroscience. Authors Dr. Paul Thompson, associate professor of neurology, and Dr. Edythe London, professor at the UCLA Neuropsychiatric Institute, are available for interviews.
A copy of the full study is available here
Other graphics related to the study can be found at http://www.loni.ucla...pson/MA/ma.html.
Journal of Neuroscience Article:
[1] Paul M. Thompson, Kiralee M. Hayashi, Sara L. Simon, Jennifer A. Geaga, Michael S. Hong, Yihong Sui, Jessica Y. Lee, Arthur W. Toga, Walter Ling, Edythe D. London (2004). Structural Abnormalities in the Brains of Human Subjects who Use Methamphetamine, Journal of Neuroscience, 24(26):6028-6036, June 30, 2004. [PDF (643 KB)] : [1] Paul M. Thompson, Kiralee M. Hayashi, Sara L. Simon, Jennifer A. Geaga, Michael S. Hong, Yihong Sui, Jessica Y. Lee, Arthur W. Toga, Walter Ling, Edythe D. London (2004). Structural Abnormalities in the Brains of Human Subjects who Use Methamphetamine, Journal of Neuroscience, 24(26):6028-6036, June 30, 2004. [PDF (643 KB)]
--------------------------------
Related Publications
Time-Lapse Maps of Brain Change in Alzheimer's Disease
Time-Lapse Movies of Brain Growth in Children and Teenagers
Time-Lapse Maps of Schizophrenia
Did you Inherit Your Brain Structure and IQ?
other research areas
(back to main list)
Contact Information
Mail:
Paul Thompson, Ph.D.
Associate Professor of Neurology
UCLA Lab of Neuro-Imaging and Brain Mapping Division
Dept. Neurology and Brain Research Institute
4238 Reed Neurology, UCLA Medical Center
710 Westwood Plaza
Westwood, Los Angeles CA 90095-1769, USA.
E-mail: thompson@loni.ucla.edu
Tel: (310)206-2101
Fax: (310)206-5518
Posted 25 January 2007 - 11:09 PM

Edited by nootropikamil, 24 March 2007 - 05:41 AM.
Posted 24 March 2007 - 05:54 PM
Alcohol 'is more dangerous than ecstacy'
Last Updated: 12:01am GMT 23/03/2007
Alcohol is ranked much more harmful than the Class A drug ecstasy in a controversial new classification system proposed by a team of leading scientists.
The table, published today in The Lancet medical journal, was drawn up by a team of highly respected experts led by Professor David Nutt, from the University of Bristol, and Professor Colin Blakemore, chief executive of the Medical Research Council.
The authors proposes that drugs should be classified by the amount of harm that they do, rather than the sharp A, B, and C divisions in the UK Misuse of Drugs Act.
They say the basis of the Act is ill-defined, opaque, and seemingly arbitrary and overestimates the risks of ecstasy, which kills around ten people annually of the half a million people who use it every weekend, while neglecting those of alcohol, a legal substance which kills more than 300 annually by acute poisoning, and many tens of thousands by road traffic accidents, cirrhosis, gut and heart disease.
In the paper, the team argues that it would make much more sense for drugs to be reclassified on a rational basis that can be updated as new evidence emerges, and more easily than the current rigid category system now in use.
Prof Blakemore added that policies of the past four decades “clearly have not worked”, given the ubiquity and low price of illegal drugs, and that fresh thinking is now required.
Today’s call to overhaul the UK drug classification system, which will be examined by the forthcoming UK Drug Policy Commission, is likely to receive popular public support, according to research into attitudes to drugs by the Academy of Medical Sciences’ DrugsFutures project.
Harmful drugs are currently regulated according to classification systems that purport to relate to the harms and risks of each drug.
However, “these are generally neither specified nor transparent, which reduces confidence in their accuracy and undermines health education messages,” said Prof Blakemore.
“The most striking observation is that there is no statistical correlation between this ranking of harm of drugs and the ABC classification.”
In the new system legal drugs, such as alcohol and nicotine, are ranked alongside illegal drugs.
The new ranking places alcohol and tobacco in the upper half of the league table. These socially accepted drugs were judged more harmful than cannabis, and substantially more dangerous than the Class A drugs LSD, 4-methylthioamphetamine and ecstasy.
“Alcohol is not far behind demonised terrors of the street such as heroin and cocaine,” said Prof Blakemore.
But the conclusions are likely to be ignored, according to coauthor Prof David Nutt from the University of Bristol, who has worked with the Advisory Council for the Misuse of Drugs.
Because some individuals with a particularly genetic make-up are at greater risk, as has been seen with rare deaths connected with ecstasy, ministers have been reluctant to change classifications despite the relative safety for the rest of the population.
Several millennia of human experience with alcohol, its pervasiveness in industrialised cultures, and the US experience with alcohol prohibition (1920–32) make it unlikely that any industrialised society will criminalise alcohol use, he said.
But that still leaves taxation and regulation as methods of control. “Alcohol is a drug we should take very seriously.”
The team identified three main factors that together determine the harm associated with any drug of potential abuse: the physical harm to the individual user caused by the drug; the tendency of the drug to induce dependence and addiction; the effect of drug use on families, communities, and society
Within each of these categories, they recognized three components, leading to a comprehensive “matrix of harm”.
Expert panels gave scores, from zero to three, for each category of harm for 20 different drugs.
All the scores for each drug were combined to produce an overall estimate of its harm. In order to provide familiar benchmarks, for comparison with illicit drugs, five legal drugs of potential misuse (alcohol, khat, solvents, alkyl nitrites, and tobacco) and one that has since been classified (ketamine) were included in the assessment. The process proved simple, and yielded roughly similar scores for drug harm when used by two separate groups of experts, one of consultant psychiatrists who were on the Royal College of Psychiatrists’ register as specialists in addiction and the second including a range of expertise, from police chief constables to scientists. “The two show very good agreement,” said Prof Nutt.
Cannabis, the subject of much recent debate, was ranked below tobacco, despite the evidence for a link with psychotic episodes in about 7% of schizophrenics. Since the expert panels were asked to assess the harm of drugs in the form that they are currently used, this ranking took account of the widespread use of skunk, which is about twice as potent than traditional cannabis resin.
Other experts still doubt there is a cause and effect relationship between cannabis and psychosis, while a study that claimed genes place some people at particular risk requires confirmation.
Prof Nutt said that young people believe that the establishment lies and distorts the dangers posed by drugs and the only way to restore their confidence is to rely on hard evidence, not arbitrary classifications.
“It is a landmark paper, a real step towards evidence based classification,” commented Prof Leslie Iversen of the University of Oxford, a member of a working group of the Academy of Medical Sciences, though he added that there is still more to be done to take on board new understanding of addiction arising from neuroscience.
The Academy has been asked by the Government to undertake an independent review of the issues raised in the Foresight report ‘DrugsFutures 2025?’ The review will take on board the opinions of many hundreds of people from across the UK who have taken part in face to face discussions and an online debate at www.drugsfutures.org.uk, which is open until end of this month.
Participants are clear that the current classification of drugs is “confusing and inconsistent”. A majority of participants support a health-based approach to drug use and treatment, rather than a law enforcement approach. Many also point out that alcohol is one of the most harmful drugs in common use, to both individuals and wider society.
There appears to be little support for decriminalising drugs however. Professor Sir Gabriel Horn, Chair of the Academy of Medical Sciences group considering the findings of the DrugsFutures project said “The UK Government have asked us to explore the likely future impact of recent developments in science on addiction, drug use and treatments for mental health. We have heard views from both members of the scientific community and of the public which indicate that the current classification system is in need of review.
“Such a review must be underpinned by evidence on the harms of drug use to the individual user, to families and to society, and be considered in the light of the latest evidence from the brain sciences.”
Drug misuse is one of the major social, legal, and public-health challenges in the modern world.
In the UK, the total burden of drug misuse, in terms of health, social, and crime-related costs, has been estimated to be between £10 billion and £16 billion per year.
Information appearing on telegraph.co.uk is the copyright of Telegraph Media Group Limited and must not be reproduced in any medium without licence. For the full copyright statement see Copyright

 --
--Edited by nootropikamil, 24 March 2007 - 06:22 PM.
Posted 24 March 2007 - 07:21 PM
Posted 28 March 2007 - 07:25 AM
Chron.com: News Source
March 27, 2007, 1:56PM
Man who recorded his meth addiction dies
By JIM SUHR Associated Press Writer
© 2007 The Associated Press
ST. LOUIS — A former trucker whose documentary chronicled an agonizing descent as methamphetamine ravaged his body has died, optimistic to the end that his story would keep others from the highly addictive stimulant.
"He was extremely satisfied, wanting to do more in getting the word out and showing kids what meth harm does. We didn't get to that point," his father, Jack Bridges, said shortly after the 35-year-old died Monday at a hospital in Cape Girardeau.
"He didn't want anyone to go through what he did," his father said.
Shawn Bridges drew global attention last year for "No More Sunsets," a 29-minute film shot by a former southern Illinois television videographer at Bridges' request.
By his family's account, Bridges already had died at least twice, his heart so damaged by years of using meth — a concoction that can include toxic chemicals such as battery acid, drain cleaner and fertilizer — that it stopped and had to be shocked back into beating.
The documentary shows Bridges mostly bedridden, his constant companions a catheter and feeding tube.
"I'd say he's got a 34-year-old body on the outside with a 70- to 80-year-old man on the inside," his father told The Associated Press last May.
About 28,000 people sought treatment for meth addiction across the country in 1993, accounting for nearly 2 percent of admissions for drug-abuse care, according to the federal Substance Abuse and Mental Health Services Administration.
A decade later, the meth-related admissions numbered nearly 136,000 — more than 7 percent of the national total for drug-abuse treatment.
Family members have said Bridges had been haunted by the dreary day in 1976 when his younger brother Jason, barely a year old, died in a car wreck. Bridges was 4 and nowhere near the accident but still blamed himself, wanting to trade places with his dead sibling, his father said.
A lenient upbringing set Bridges on the road to becoming "a little monster," his father said. "By 16, the kid was a high school dropout and partier."
At 26, Bridges had a heart attack that his father blamed on meth's ability to damage a chronic user's heart and other internal organs. Bridges learned he had congestive heart failure. Twice, he tried to kill himself, family members said.
During his final months in a hospital bed, Bridges' words slurred to guttural sounds. At times, he spit up blood, and his weight fell dangerously when he couldn't keep food down. His father said Monday that Bridges developed a urinary tract infection shortly before he died.
"I don't think people will forget what got him to this point," said Chip Rossetti, who filmed the documentary. "But what he did with his condition is really the amazing thing."
Rossetti said 500 to 600 copies of the documentary have been sold, some going as far as Australia. Bridges was also profiled on German television. Rossetti said Monday he plans a sequel, chronicling Bridge's final year and testimonials by people touched by his awareness effort.
"We wanted to keep him with us a lot longer, but we appreciate God's good grace," Jack Bridges said. "We'll still be trying to drive home the point that these drugs are poison, and that people using them are heading the same place Shawn has gone."
___
On the Net:
Partnership for a Drug-Free America: http://www.drugfree.org/Meth
Posted 29 March 2007 - 04:17 AM
Posted 29 March 2007 - 04:27 AM
Posted 29 March 2007 - 04:49 AM
I wouldn't call this just a pop science media report.
SANDRA BLAKESLEE
NEW YORK TIMES
People who do not want to wait for old age to shrink their brains and bring on memory loss now have a quicker alternative — abuse methamphetamine for a decade or so and watch the brain cells vanish into the night.
The first high-resolution MRI study of methamphetamine addicts shows "a forest fire of brain damage," said Dr. Paul Thompson, an expert on brain mapping at the University of California, Los Angeles. "We expected some brain changes but didn't expect so much tissue to be destroyed."
The image, published in the June 30 issue of The Journal Of Neuroscience, shows the brain's surface and deeper limbic system. Red areas show the greatest tissue loss.
The limbic region, involved in drug craving, reward, mood and emotion, lost 11 per cent of its tissue.
"The cells are dead and gone," Thompson said.
Addicts were depressed, anxious and unable to concentrate.
The brain's centre for making new memories, the hippocampus, lost 8 per cent of its tissue, comparable to the brain deficits in early Alzheimer's. The methamphetamine addicts fared significantly worse on memory tests than healthy people the same age.
The study examined 22 people in their 30s who had used methamphetamine for 10 years, mostly by smoking it, and 21 controls matched for age.
On average, the addicts used four grams a week and said they had been high on 19 of the 30 days before the study began.
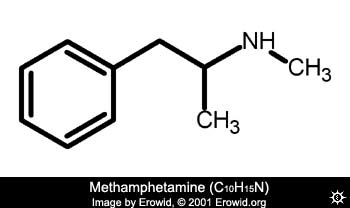
Methamphetamine is an addictive stimulant made in clandestine laboratories throughout North America. When taken by mouth, snorted, injected or smoked, it produces intense pleasure by releasing the brain's reward chemical, dopamine.
With chronic use, the brains that overstimulate dopamine and another brain chemical, serotonin, are permanently compromised.
The study held one other surprise, Thompson said.
White matter, composed of nerve fibres that connect different areas, was severely inflamed, making the addicts' brains 10 per cent larger than normal.
"This was shocking," he said.
But there was one piece of good news. The white matter was not dead. With abstinence, it might recover.
Posted 29 March 2007 - 04:10 PM
Posted 29 March 2007 - 05:04 PM
This quote references the Wilson (1996) that I linked to above, as well as some more recent papers [papers as recent as the one you linked to].However, striatal concentrations of one marker, the vesicular monoamine transporter (VMAT2), considered to be a somewhat more ‘stable’ marker of striatal dopamine nerve terminal integrity (Vander Borght et al., 1995; Wilson and Kish 1996; but see Riddle et al., 2002 and de la Fuente-Fernández et al., 2003), are normal in postmortem brain of MA users (Wilson et al., 1996a) whereas in living brain of self-reported MA users (using PET) VMAT2 levels are, at most, only slightly reduced (personal communication, C. Schuster and C.-E. Johanson, Wayne State University, Detroit MI; K. Frey, University of Michigan, Ann Arbor MI). These data suggest that striatal dopamine nerve terminal number might not be substantially decreased in human MA users.
http://brain.oxfordj.../full/127/2/363
As for the Thompson et al. (2004) paper you linked to, I have a couple comments on it:Dopa-responsive dystonia (DRD) is a lifelong disorder in which dopamine deficiency is not associated with neuronal loss and therefore it is an ideal human model for investigating the compensatory changes that occur in response to this biochemical abnormality. Using positron emission tomography (PET), we examined the (+/-)-alpha-[(11)C]dihydrotetrabenazine ([(11)C]DTBZ) binding potential of untreated DRD patients and normal controls. Two other PET markers of presynaptic nigrostriatal function, d-threo-[(11)C]methylphenidate ([(11)C]MP) and 6-[(18)F]fluoro-L-dopa ([(18)F]-dopa), and [(11)C]raclopride were also used in the study. We found increased [(11)C]DTBZ binding potential in the striatum of DRD patients. By contrast, no significant changes were detected in either [(11)C]MP binding potential or [(18)F]-dopa uptake rate constant. In addition, we found evidence for increased dopamine turnover in one DRD patient by examining changes in [(11)C]raclopride binding potential in relation to levodopa treatment. We propose that the increase in [(11)C]DTBZ binding likely reflects the dramatic decrease in the intravesicular concentration of dopamine that occurs in DRD; upregulation of vesicular monoamine transporter type 2 (VMAT2) expression may also contribute. Our findings suggest that the striatal expression of VMAT2 (as estimated by [(11)C]DTBZ binding) is not coregulated with dopamine synthesis. This is in keeping with a role for VMAT2 in other cellular processes (i.e., sequestration and release from the cell of potential toxic products), in addition to its importance for the quantal release of monoamines.
http://www.ncbi.nlm....t_uids=12710012
Edited by mr_kite, 29 March 2007 - 05:23 PM.
Posted 29 March 2007 - 09:34 PM
Luv2increase, I wouldn't mind showing you at all. Also, I called it pop science because it was in the New York Times. If you would have cited the original paper from the start, then it wouldn't have been accurate for me to say that. But you didn't. Most pop science has references somewhere, but careful reading of those references does not always yeild the same conclusion as the one presented in the pop science presentation of those references. (luv2increase, I have seen you around mind and muscle. I have posted there on various aspects of the DA systems)
syndication
Definition
The supplying of information or content for simultaneous publication in several periodicals or web sites.
July 20, 2004
This Is Your Brain on Meth: A 'Forest Fire' of Damage
By SANDRA BLAKESLEE
People who do not want to wait for old age to shrink their brains and bring on memory loss now have a quicker alternative -- abuse methamphetamine for a decade or so and watch the brain cells vanish into the night.
The first high-resolution M.R.I. study of methamphetamine addicts shows ''a forest fire of brain damage,'' said Dr. Paul Thompson, an expert on brain mapping at the University of California, Los Angeles. ''We expected some brain changes but didn't expect so much tissue to be destroyed.''
The image, published in the June 30 issue of The Journal of Neuroscience, shows the brain's surface and deeper limbic system. Red areas show the greatest tissue loss.
The limbic region, involved in drug craving, reward, mood and emotion, lost 11 percent of its tissue. ''The cells are dead and gone,'' Dr. Thompson said. Addicts were depressed, anxious and unable to concentrate.
The brain's center for making new memories, the hippocampus, lost 8 percent of its tissue, comparable to the brain deficits in early Alzheimer's. The methamphetamine addicts fared significantly worse on memory tests than healthy people the same age.
The study examined 22 people in their 30's who had used methamphetamine for 10 years, mostly by smoking it, and 21 controls matched for age. On average, the addicts used an average of four grams a week and said they had been high on 19 of the 30 days before the study began.
Methamphetamine is an addictive stimulant made in clandestine laboratories nationwide. When taken by mouth, snorted, injected or smoked, it produces intense pleasure by releasing the brain's reward chemical, dopamine. With chronic use, the brains that overstimulate dopamine and another brain chemical, serotonin, are permanently compromised.
The study held one other surprise, Dr. Thompson said: white matter, composed of nerve fibers that connect different areas, was severely inflamed, making the addicts' brains 10 percent larger than normal. ''This was shocking,'' he said. But there was one piece of good news: the white matter was not dead. With abstinence, it might recover.
June 11, 2005
Grisly Effect of One Drug: 'Meth Mouth'
By MONICA DAVEY
From the moment on Thursday when the young man sat down in Dr. Richard Stein's dental chair in southwestern Kansas and opened his mouth, Dr. Stein was certain he recognized the enemy. This had to be the work, he concluded, of methamphetamine, a drug that is leaving its mark, especially in the rural regions of the Midwest and the South, on families, crime rates, economies, legislatures - and teeth.
Quite distinct from the oral damage done by other drugs, sugar and smoking, methamphetamine seems to be taking a unique, and horrific, toll inside its users' mouths. In short stretches of time, sometimes just months, a perfectly healthy set of teeth can turn a grayish-brown, twist and begin to fall out, and take on a peculiar texture less like that of hard enamel and more like that of a piece of ripened fruit.
The condition, known to some as meth mouth, has been studied little in dentistry's academic circles and is unknown to many dentists, whose patients are increasingly focused on cosmetic issues: the bleaching and perfect veneers of television's makeover shows. But other dentists, especially those in the open, empty swaths of land where methamphetamine is being manufactured in homemade laboratories, say they are seeing a growing number of such cases.
These are the same towns, in some cases, that have wrestled in recent years with shortages of dentists. They are places where dentists have struggled to sell their practices as populations shrink; where new dentists have been reluctant to settle, out of fear that they will not get enough business to make ends meet; and where political leaders have offered financial incentives to lure young dentists to town. For good or ill, meth mouth is creating more business.
East of Dr. Stein's Dodge City office, in Independence, Kan., Dr. Cynthia E. Sherwood said she too had seen such patients lately, including a woman whose teeth had been transformed into "little black stubs" too painful to brush and who wound up losing all her top teeth and six of her lower ones. Among similar patients Dr. Charles Tatlock has seen in his New Mexico office, he said, was one who, though only 17, needed dentures to replace his suddenly decayed teeth.
And in Tennessee, Dr. Daniel D. Roberts gave up his ordinary practice not long ago to handle a growing workload at 10 jails across the state, nearly a third of whose prisoners, he estimates, have ravaged teeth owing to methamphetamine.
"This is the worst thing to come along in a long time," Dr. Roberts said the other day. "At this point, I'm digging for roots. That's how I make my living."
Some dentists have their own hypotheses about precisely what causes the condition.
Dr. John W. Shaner, an associate professor at the Creighton University Medical Center School of Dentistry, in Omaha, said he believed that a combination of factors tied to the use of methamphetamine led to such enormous damage.
The drug itself, a synthetic stimulant that can be manufactured just about anywhere, causes dry mouth, Dr. Shaner said, and that in turn allows decay to start, since saliva is unavailable to help control bacteria in the mouth. The drug also tends to leave users thirsty and craving a constant supply of soda pop and other sugary drinks, which spur the decay; Mountain Dew, he said, has become the preferred drink of methamphetamine users. At the same time, the drug's highly addictive nature causes many users simply to stop doing what is needed to take care of themselves, including the brushing of teeth.
Other dentists said they suspected that the caustic ingredients of the drug - whether smoked, injected, snorted or eaten - contributed to the damage, which tends to start near the gums and wander to the edges of teeth. Among ingredients that can be used to make meth are red phosphorus found in the strips on boxes of matches and lithium from car batteries.
There are also dentists who point to methamphetamine users' tendency to grind and clench their teeth nervously, aggravating the frighteningly twisted and tangled look of meth mouth.
If the man sitting in Dr. Stein's Kansas office on Thursday, who readily admitted having used methamphetamine, gets all the work done that he needs - X-rays, fillings and crowns, and implants for the teeth now missing from his mouth - he will require many visits, and the bill could run to as much as $7,000.
Most dentists, though, say this is hardly the growth industry any of them would wish for. The patients are grim, their teeth grimmer. Many of these young people, the dentists say, may end up with no teeth at all but with dentures, which some in dentistry had come to believe would soon be mostly relics of the past, even for the elderly, in an age of water fluoridation and other technology.
"The real market for dentistry is in saving teeth, in helping people have dental health," said Dr. Stein, 57. "But I've seen a lot. I'm not a drug counselor, and I'm long past lecturing, but this is a sorry situation."
Dr. Shaner said meth mouth might be little recognized in many places - even as the drug has spread from one coast to the other and from rural areas into cities - because methamphetamine is a problem that has had a chance to sink in longer in places like Nebraska, Iowa and Missouri and because the effects to teeth are often most obvious in pockets like prison populations. He said he hoped to present information on the topic at a conference of the American Dental Association next year.
With the exception of a few formal studies, including one now beginning in New Mexico, meth mouth has so far been less a topic of academic analysis in the dental profession than a matter for casual phone conversations and e-mail exchanges between dentists in small places.
"The truth is, very little is known yet," said Dr. Stephen Wagner, who specializes in dentures and implants in his private practice and who in coming months will be studying 20 afflicted patients with Dr. Tatlock, an assistant professor at the University of New Mexico. "What I can tell you is what I have seen: It looks like someone has taken a hammer to these teeth and shattered them."
One of the strangest truths of the condition, dentists said, is that despite the truly grisly look, many patients do not report suffering from as much pain as one would expect. Or at least, these dentists said, they do not report such pain while still using methamphetamine.
Though the condition has begun turning up in private practices, particularly in cases of emergency care and among recovering addicts, it is far more prevalent in the dental offices of the nation's jails and prisons.
Local sheriffs in Midwestern and Southern counties have complained of soaring dental costs in their jails. In North Dakota, more dentures have been needed in the state penitentiary in the last few years, a development that officials attribute at least in part to methamphetamine. In North Carolina, dental workers in the Department of Correction learned about meth mouth during a training session this month; starting in July, new prisoners there will be screened for signs of dental problems connected to the drug.
In Minnesota's state corrections system, meanwhile, dentists' workloads are so full of gruesome methamphetamine-related matters that they are strained to get to other, less urgent cases: the routine cleanings and fillings of years past.
"All of our time is getting eaten up," said Dr. Stephen Boesch, a dentist who works at a Minnesota prison and who said he had begun to see the problem in a juvenile corrections center as well. "We're seeing this week in and week out."
Some dentists said they would never ask their patients about drug use; that is not their place, they said. Others said they would ask, but could not force the issue.
"That's the thing: you can't beat a confession from someone," said Dr. Eric Curtis, who shares a practice with his father in Safford, Ariz., and began seeing meth mouth four years ago.
"I suspect that many dentists are out there seeing this but don't know what they're seeing," said Dr. Curtis, a spokesman for the Academy of General Dentistry. "And most of them aren't going to know for sure."
The new business, he said, is actually a gloomy one for dentists in rural places like Safford.
"What dentists really make the money on is the happy stuff: the low-impact work with beautiful results," he said. "Nobody is happy when you pull a bunch of teeth and put in dentures."
Gretchen Ruethling contributed reporting for this article.
March 27, 2007
Man Who Recorded His Meth Addiction Dies
By THE ASSOCIATED PRESS
Filed at 4:14 p.m. ET
ST. LOUIS (AP) -- A former trucker whose documentary chronicled an agonizing descent as methamphetamine ravaged his body has died, optimistic to the end that his story would keep others from the highly addictive stimulant.
''He was extremely satisfied, wanting to do more in getting the word out and showing kids what meth harm does. We didn't get to that point,'' his father, Jack Bridges, said shortly after the 35-year-old died Monday at a hospital in Cape Girardeau.
''He didn't want anyone to go through what he did,'' his father said.
Shawn Bridges drew global attention last year for ''No More Sunsets,'' a 29-minute film shot by a former southern Illinois television videographer at Bridges' request.
By his family's account, Bridges already had died at least twice, his heart so damaged by years of using meth -- a concoction that can include toxic chemicals such as battery acid, drain cleaner and fertilizer -- that it stopped and had to be shocked back into beating.
The documentary shows Bridges mostly bedridden, his constant companions a catheter and feeding tube.
''I'd say he's got a 34-year-old body on the outside with a 70- to 80-year-old man on the inside,'' his father told The Associated Press last May.
About 28,000 people sought treatment for meth addiction across the country in 1993, accounting for nearly 2 percent of admissions for drug-abuse care, according to the federal Substance Abuse and Mental Health Services Administration.
A decade later, the meth-related admissions numbered nearly 136,000 -- more than 7 percent of the national total for drug-abuse treatment.
Family members have said Bridges had been haunted by the dreary day in 1976 when his younger brother Jason, barely a year old, died in a car wreck. Bridges was 4 and nowhere near the accident but still blamed himself, wanting to trade places with his dead sibling, his father said.
A lenient upbringing set Bridges on the road to becoming ''a little monster,'' his father said. ''By 16, the kid was a high school dropout and partier.''
At 26, Bridges had a heart attack that his father blamed on meth's ability to damage a chronic user's heart and other internal organs. Bridges learned he had congestive heart failure. Twice, he tried to kill himself, family members said.
During his final months in a hospital bed, Bridges' words slurred to guttural sounds. At times, he spit up blood, and his weight fell dangerously when he couldn't keep food down. His father said Monday that Bridges developed a urinary tract infection shortly before he died.
''I don't think people will forget what got him to this point,'' said Chip Rossetti, who filmed the documentary. ''But what he did with his condition is really the amazing thing.''
Rossetti said 500 to 600 copies of the documentary have been sold, some going as far as Australia. Bridges was also profiled on German television. Rossetti said Monday he plans a sequel, chronicling Bridge's final year and testimonials by people touched by his awareness effort.
''We wanted to keep him with us a lot longer, but we appreciate God's good grace,'' Jack Bridges said. ''We'll still be trying to drive home the point that these drugs are poison, and that people using them are heading the same place Shawn has gone.''
------
On the Net:
Partnership for a Drug-Free America: http://www.drugfree.org/Meth
Nootropikamil, my primary source for those comments are the lectures given by Professor Anagnostaras in my Drugs & Behavior class at UCSD (Psych 181). I believe you went to UCSD as well, but I am not sure if you have taken this course or even heard of it.
Neuropharmacology. 2004;47 Suppl 1:92-100.
The methamphetamine experience: a NIDA partnership.
Hanson GR, Rau KS, Fleckenstein AE.
Department of Pharmacology and Toxicology, University of Utah, 30 South 2000 East, Skaggs Hall, Room 112, Salt Lake City, UT 84112, USA. glen.hanson@hsc.utah.edu
The neurotoxic properties of the amphetamines such as methamphetamine (METH) were originally described about the time of the National Institute on Drug Abuse's organization, in the early 1970s. It required more than 20 years to confirm these neurotoxic properties in humans. Much like Parkinson's disease, multiple high-dose administration of METH somewhat selectively damages the nigrostriatal dopamine (DA) projection of the brain. This effect appears to be related to the intracellular accumulation of cytosolic DA and its ability to oxidize into reactive oxygen species. Both the dopamine plasmalemmal transporter and the vesicular monoamine transporter-2 seem to play critical roles in this neurotoxicity. METH and related analogs such as methylenedioxymethamphetamine (MDMA) can also damage selective CNS serotonin neurons. The mechanism of the serotonergic neurotoxicity is not as well characterized, but also appears to be related to the formation of reactive oxygen species and monoamine transporters. Studies examining the pharmacological and neurotoxicological properties of the amphetamines have helped to elucidate some critical features of monoamine regulations as well as helped to improve our understanding of the processes associated with degenerative disorders such as Parkinson's disease.
Publication Types:
Review
PMID: 15464128 [PubMed - indexed for MEDLINE]
Nihon Shinkei Seishin Yakurigaku Zasshi. 2002 Apr;22(2):35-47.
[A recent trend in methamphetamine-induced neurotoxicity]
[Article in Japanese]
Kita T, Nakashima T.
Department of Pharmacology, Nara Medical University.
The neurotoxic damage caused by methamphetamine (METH) is characterized by nerve terminal destruction and/or degeneration of the dopaminergic and serotonergic systems in striatum and hippocampus. It has been hypothesized that intraneural dopamine (DA) redistribution from synaptic vesicles to cytoplasmic compartments produced by METH is an important factor for its neurotoxicity. The METH-induced redistribution of DA is thought to occur after an increased production of DA-based reactive oxygen species (ROS) (e.g., oxygen radicals and hydroxyl radicals) by auto-oxidation or enzymatic degradation, and METH-induced ROS produces an oxidative stress and depletion of energy stores. Furthermore, the glutamatergic system and nitric oxide (NO) may also contribute to METH-induced neurotoxicity. Recently, studies using several knockout strains of mice lacking the DA transporter, the monoamine vesicle transporter-2, c-fos, or neuronal NO synthase confirm a possible role of these factors in METH-induced neurotoxicity. Moreover, it has been proposed that METH causes the apoptosis and activation of cell-death-related genes. For example, METH-induced neurotoxicity is reduced in bcl-2-over expressing neural cell and p53 knockout mice and also induces the activation of caspase 3. Therefore in this review, we discuss the relationship between ROS formation, oxidative stress, and apoptosis in METH-induced neurotoxicity.
Publication Types:
Review
Review, Tutorial
Ann N Y Acad Sci. 2004 Oct;1025:162-70.
Similarities between methamphetamine toxicity and proteasome inhibition.
Fornai F, Lenzi P, Gesi M, Ferrucci M, Lazzeri G, Capobianco L, de Blasi A, Battaglia G, Nicoletti F, Ruggieri S, Paparelli A.
Department of Human Morphology and Applied Biology, University of Pisa, Pisa, Italy. f.fornai@med.unipi.it
The monoamine neurotoxin methamphetamine (METH) is commonly used as an experimental model for Parkinson's disease (PD). In fact, METH-induced striatal dopamine (DA) loss is accompanied by damage to striatal nerve endings arising from the substantia nigra. On the other hand, PD is characterized by neuronal inclusions within nigral DA neurons. These inclusions contain alpha-synuclein, ubiquitin, and various components of a metabolic pathway named the ubiquitin-proteasome (UP) system, while mutation of genes coding for various components of the UP system is responsible for inherited forms of PD. In this presentation we demonstrate for the first time the occurrence of neuronal inclusions in vivo in the nigrostriatal system of the mouse following administration of METH. We analyzed, in vivo and in vitro, the shape and the fine structure of these neuronal bodies by using transmission electron microscopy. Immunocytochemical investigation showed that these METH-induced cytosolic inclusions stain for ubiquitin, alpha-synuclein, and UP-related molecules, thus sharing similar components with Lewy bodies occurring in PD, with an emphasis on enzymes belonging to the UP system. In line with this, blockade of this multicatalytic pathway by the selective inhibitor epoxomycin produced cell inclusions with similar features. Moreover, using a multifaceted pharmacological approach, we could demonstrate the need for endogenous DA in order to form neuronal inclusions.
PMID: 15542714 [PubMed - indexed for MEDLINE]
Edited by nootropikamil, 29 March 2007 - 09:47 PM.
Posted 29 March 2007 - 11:50 PM
I do not believe I have stated that MA cannot cause neurotoxicity. I agree with you, in that it can cause neurotoxicity and there are many well known papers that show this (which you are likely to be aware of based on the pubmed searching you have already done). The important questions are:The evidence for neurotoxicity from methamphetamine abuse isn't anything new.
In the news industry, I learned there is a little something called syndication
...
It appears that the New York Times is quite a popular newspaper!
...
I don't doubt that Dr. Anagnostaras is a qualified neuroscientist or an excellent professor. I checked Dr. Anagnostaras's CV -- it's quite impressive! However, I don't really see any "hands on" experience that Dr. Anagnostaras has in the laboratory with methamphetamine.
I believe Dr. Anagnostaras might be trying to teach you how to think critically and like a scientist and it appears he's done his job! You're out there already checking study designs! He must be a great professor -- he also happens to teach at UCSD -- a great university!
...
Mr. Kite: keep in mind that we're here to help you!
I wanted to note that, as requested in your signature, you were very rude and condescending in your post (specifically in the excerpts quoted above). It is hard to reply to perceived ad hominem's without resorting to them yourself; so with that in mind, I'll reply to your post as best I can and space out my reply and make each point one by one so you can follow easier.NOTE: I try to make my Internet posts accurate; however, some thoughts I post here may not be. If you feel anything I wrote is incorrect or rude, please notify me how and I might change it.
I have read about that incident, but that does not engage the four questions I listed above.I recall once when my brother schooled me (an educational 'bitch slap' of sorts
) once about fraud frequently happens in science due to financial, political, and other miscellaneous sorts of conflicts of interest. He provided an example from a well known study that supposedly "proved" the neurotoxicity of MDMA ("ecstasy"). The researcher used methamphetamine (which is a well established neurotoxin) instead of MDMA. So when that researcher was busted using meth instead of ex, he was forced to retract the findings.
Posted 30 March 2007 - 07:29 PM
I do not believe I have stated that MA cannot cause neurotoxicity. I agree with you, in that it can cause neurotoxicity and there are many well known papers that show this (which you are likely to be aware of based on the pubmed searching you have already done). The important questions are:The evidence for neurotoxicity from methamphetamine abuse isn't anything new.
(1) At what dosage does MA cause synaptic degeneration?
(2) At what dosage does MA cause neuronal death?
(3) Are these dosages used by addicts?
(4) What factor does chronic use play? There will be different answers to the three previous questions depending on whether we speak in terms of acute doses or chronic doses.
In the news industry, I learned there is a little something called syndication
...
It appears that the New York Times is quite a popular newspaper!
...
I don't doubt that Dr. Anagnostaras is a qualified neuroscientist or an excellent professor. I checked Dr. Anagnostaras's CV -- it's quite impressive! However, I don't really see any "hands on" experience that Dr. Anagnostaras has in the laboratory with methamphetamine.
I believe Dr. Anagnostaras might be trying to teach you how to think critically and like a scientist and it appears he's done his job! You're out there already checking study designs! He must be a great professor -- he also happens to teach at UCSD -- a great university!
...
Mr. Kite: keep in mind that we're here to help you!
NOTE: I try to make my Internet posts accurate; however, some thoughts I post here may not be. If you feel anything I wrote is incorrect or rude, please notify me how and I might change it.
I wanted to note that, as requested in your signature, you were very rude and condescending in your post (specifically in the excerpts quoted above). It is hard to reply to perceived ad hominem's without resorting to them yourself; so with that in mind, I'll reply to your post as best I can and space out my reply and make each point one by one so you can follow easier.
First, you were being sarcastic when you were talking about syndication and the NYT, right? I really don't believe that you thought I was unaware of this. What I meant by my use of the term 'pop science' is anything that has been reinterpreted for the lay and published in a non-'peer reviewed' journal/paper/website. The best source for scientific information is original research published in peer reviewed journals, and review papers published in peer reviewed journals. The article that I was referring to originally when talking about DAT vs. VMAT (now that I look back) was the PBS Frontline article in the first post, not the NYT (even though the NYT counts as well). I may be using the term 'pop science' in a way that is broader than you thought I was, but your comment was still out of line.
Using a measure of DAT levels is not a good indicator of synaptic damage or degeneration. DAT levels are down regulated in the same way that postsynaptic DA receptors are. A measure of VMAT levels is more indicative of whether there has been actual degeneration. Studies have been done on methamphetamine users and they do not show significant losses in VMAT. So while there is down regulation in the functionality of the neurons, there isn't much evidence to show actual synaptic degeneration or neuronal death. This is especially true at the doses that methamphetamine users take. The doses that are used in rats to cause neurotoxicity are much higher than the actual street doses (unlike, for example, MDMA, where the street dose is neurotoxic).
A better place to get information are published journal articles, not pop science media reports and testimonials from sites trying to lower meth use.
Second, the CV of the professor teaching a class is not very relevant, ceteris paribus, to their ability to read the required papers to be covered within the scope of a class and then organize a series of lectures on the basis of those papers. One does not need to work in a lab with methamphetamine in order to lecture on methamphetamine, for example.
Third, you imply that I have learned a lot from this particular professor and that I like him (I guess thats what you were getting at). In fact, I haven't learned much from him. Rather, I have had many other classes and experience in a lab which have all contributed to my ability to analyze research designs and design my own experiments. What was the point of this section of your post? I merely noted the class title in case you had taken it, there were no appeals to authority on my part. I cited not only the original lecture materials that the information came from, but also the papers referenced to in those lectures.
Fourth, you are here to help me? I don't know what you intended by this or were trying to imply, but I won't make any assumptions. I'll only request that you not make paternalistic statements regarding me in the future.
I recall once when my brother schooled me (an educational 'bitch slap' of sorts
) once about fraud frequently happens in science due to financial, political, and other miscellaneous sorts of conflicts of interest. He provided an example from a well known study that supposedly "proved" the neurotoxicity of MDMA ("ecstasy"). The researcher used methamphetamine (which is a well established neurotoxin) instead of MDMA. So when that researcher was busted using meth instead of ex, he was forced to retract the findings.
I have read about that incident, but that does not engage the four questions I listed above.
The rest of the papers you quoted do not disagree with what I have said in this post. It is important that you see why this is, because if you miss this, then we will be talking past each other for the rest of the discussion.
Keep in mind that my original post was in disagreement with the section of the first post saying: "Brain images of a person who has never used methamphetamine (left) and of a methamphetamine user after 1 month of abstinence (center). Lighter colors show distribution of dopamine transporters (DAT) in the striatum. DAT distribution is reduced in striatum of methamphetamine user. Brain image of a methamphetamine user after 14 months' abstinence (right) shows substantial recovery of DAT in striatum. Low levels of DAT in methamphetamine users were associated with poorer performance on tests of memory and motor skills, which did not improve with DAT after lengthy abstinence." Then my second post was providing references for the assertions made in my first post, and then I took a look at the MRI study showing a loss of gray-matter.
In response to the four questions I posed above; I maintain that the dosages used by most addicts are insufficient in themselves to cause synaptic degradation or neuronal death in humans. Evidence in favor of this view can be found in the Wilson (1996) paper and the Wilson paper is corroborated by the de la Fuente-Fernández et al. (2003) paper.
For now I will assume that you misinterpreted my original post and intended no harm (despite some anger that may have slipped through in this reply). Otherwise, I will not engage in an ad hominem laced debate in which the two debaters talk past each other (as I have seen happen on this forum before).
Edited by nootropikamil, 30 March 2007 - 11:02 PM.
Posted 03 April 2007 - 11:44 PM
Since I, in fact, did cite the references previously, I will now quote myself and spell it out for you.I'm not sure, but I didn't see a shred of evidence supporting any your points in your first post in this topic; meanwhile you dismiss other fine journalists' work as "pop science."
Using a measure of DAT levels is not a good indicator of synaptic damage or degeneration. DAT levels are down regulated in the same way that postsynaptic DA receptors are. A measure of VMAT levels is more indicative of whether there has been actual degeneration. Studies have been done on methamphetamine users and they do not show significant losses in VMAT. So while there is down regulation in the functionality of the neurons, there isn't much evidence to show actual synaptic degeneration or neuronal death. This is especially true at the doses that methamphetamine users take. The doses that are used in rats to cause neurotoxicity are much higher than the actual street doses (unlike, for example, MDMA, where the street dose is neurotoxic).
From the powerpoint lecture on amphetamines (which I can link to: http://psy.ucsd.edu/...os/181lec6.ppt), he references this paper - Wilson (1996): http://www.nature.co....861158020.html, or http://www.ncbi.nlm....st_uids=8640565 for the pubmed version
That is, the found that DAT went down in MA abusers, but VMAT (which is known to be reduced in parkisonian patients, who have synaptic degeneration) was not reduced.We found reduced levels of three dopamine nerve terminal markers (dopamine, tyrosine hydroxylase and the dopamine transporter) in post-mortem striatum (nucleus accumbens, caudate, putamen) of chronic methamphetamine users. However, levels of DOPA decarboxylase and the vesicular monoamine transporter, known to be reduced in Parkinson's disease were normal. This suggests that chronic exposure to methamphetamine does not cause permanent degeneration of striatal dopamine nerve terminals at the doses used by the young subjects in our study.
http://www.nature.co....861158020.html
This reiterates what was found by Wilson (1996), and adds to it, showing results from living MA abusers as well.However, striatal concentrations of one marker, the vesicular monoamine transporter (VMAT2), considered to be a somewhat more ‘stable’ marker of striatal dopamine nerve terminal integrity (Vander Borght et al., 1995; Wilson and Kish 1996; but see Riddle et al., 2002 and de la Fuente-Fernández et al., 2003), are normal in postmortem brain of MA users (Wilson et al., 1996a) whereas in living brain of self-reported MA users (using PET) VMAT2 levels are, at most, only slightly reduced (personal communication, C. Schuster and C.-E. Johanson, Wayne State University, Detroit MI; K. Frey, University of Michigan, Ann Arbor MI). These data suggest that striatal dopamine nerve terminal number might not be substantially decreased in human MA users.
http://brain.oxfordj.../full/127/2/363
The important part here is that regulation of DA synthesis does not regulate VMAT, showing the independence of the two processes.Dopa-responsive dystonia (DRD) is a lifelong disorder in which dopamine deficiency is not associated with neuronal loss and therefore it is an ideal human model for investigating the compensatory changes that occur in response to this biochemical abnormality. Using positron emission tomography (PET), we examined the (+/-)-alpha-[(11)C]dihydrotetrabenazine ([(11)C]DTBZ) binding potential of untreated DRD patients and normal controls. Two other PET markers of presynaptic nigrostriatal function, d-threo-[(11)C]methylphenidate ([(11)C]MP) and 6-[(18)F]fluoro-L-dopa ([(18)F]-dopa), and [(11)C]raclopride were also used in the study. We found increased [(11)C]DTBZ binding potential in the striatum of DRD patients. By contrast, no significant changes were detected in either [(11)C]MP binding potential or [(18)F]-dopa uptake rate constant. In addition, we found evidence for increased dopamine turnover in one DRD patient by examining changes in [(11)C]raclopride binding potential in relation to levodopa treatment. We propose that the increase in [(11)C]DTBZ binding likely reflects the dramatic decrease in the intravesicular concentration of dopamine that occurs in DRD; upregulation of vesicular monoamine transporter type 2 (VMAT2) expression may also contribute. Our findings suggest that the striatal expression of VMAT2 (as estimated by [(11)C]DTBZ binding) is not coregulated with dopamine synthesis. This is in keeping with a role for VMAT2 in other cellular processes (i.e., sequestration and release from the cell of potential toxic products), in addition to its importance for the quantal release of monoamines.
http://www.ncbi.nlm....t_uids=12710012
Posted 03 April 2007 - 11:57 PM
Posted 05 April 2007 - 04:56 AM
You are right that my first post was poorly worded and prone to misinterpretation, and that it was out of line as well.
Since I, in fact, did cite the references previously, I will now quote myself and spell it out for you.I'm not sure, but I didn't see a shred of evidence supporting any your points in your first post in this topic; meanwhile you dismiss other fine journalists' work as "pop science."
Here is my claim in the first post:Using a measure of DAT levels is not a good indicator of synaptic damage or degeneration. DAT levels are down regulated in the same way that postsynaptic DA receptors are. A measure of VMAT levels is more indicative of whether there has been actual degeneration. Studies have been done on methamphetamine users and they do not show significant losses in VMAT. So while there is down regulation in the functionality of the neurons, there isn't much evidence to show actual synaptic degeneration or neuronal death. This is especially true at the doses that methamphetamine users take. The doses that are used in rats to cause neurotoxicity are much higher than the actual street doses (unlike, for example, MDMA, where the street dose is neurotoxic).
In my second post I wrote:
Now, to quote from the Wilson (1996) study:That is, the found that DAT went down in MA abusers, but VMAT (which is known to be reduced in parkisonian patients, who have synaptic degeneration) was not reduced.We found reduced levels of three dopamine nerve terminal markers (dopamine, tyrosine hydroxylase and the dopamine transporter) in post-mortem striatum (nucleus accumbens, caudate, putamen) of chronic methamphetamine users. However, levels of DOPA decarboxylase and the vesicular monoamine transporter, known to be reduced in Parkinson's disease were normal. This suggests that chronic exposure to methamphetamine does not cause permanent degeneration of striatal dopamine nerve terminals at the doses used by the young subjects in our study.
http://www.nature.co....861158020.htmlThis reiterates what was found by Wilson (1996), and adds to it, showing results from living MA abusers as well.However, striatal concentrations of one marker, the vesicular monoamine transporter (VMAT2), considered to be a somewhat more ‘stable’ marker of striatal dopamine nerve terminal integrity (Vander Borght et al., 1995; Wilson and Kish 1996; but see Riddle et al., 2002 and de la Fuente-Fernández et al., 2003), are normal in postmortem brain of MA users (Wilson et al., 1996a) whereas in living brain of self-reported MA users (using PET) VMAT2 levels are, at most, only slightly reduced (personal communication, C. Schuster and C.-E. Johanson, Wayne State University, Detroit MI; K. Frey, University of Michigan, Ann Arbor MI). These data suggest that striatal dopamine nerve terminal number might not be substantially decreased in human MA users.
http://brain.oxfordj.../full/127/2/363The important part here is that regulation of DA synthesis does not regulate VMAT, showing the independence of the two processes.Dopa-responsive dystonia (DRD) is a lifelong disorder in which dopamine deficiency is not associated with neuronal loss and therefore it is an ideal human model for investigating the compensatory changes that occur in response to this biochemical abnormality. Using positron emission tomography (PET), we examined the (+/-)-alpha-[(11)C]dihydrotetrabenazine ([(11)C]DTBZ) binding potential of untreated DRD patients and normal controls. Two other PET markers of presynaptic nigrostriatal function, d-threo-[(11)C]methylphenidate ([(11)C]MP) and 6-[(18)F]fluoro-L-dopa ([(18)F]-dopa), and [(11)C]raclopride were also used in the study. We found increased [(11)C]DTBZ binding potential in the striatum of DRD patients. By contrast, no significant changes were detected in either [(11)C]MP binding potential or [(18)F]-dopa uptake rate constant. In addition, we found evidence for increased dopamine turnover in one DRD patient by examining changes in [(11)C]raclopride binding potential in relation to levodopa treatment. We propose that the increase in [(11)C]DTBZ binding likely reflects the dramatic decrease in the intravesicular concentration of dopamine that occurs in DRD; upregulation of vesicular monoamine transporter type 2 (VMAT2) expression may also contribute. Our findings suggest that the striatal expression of VMAT2 (as estimated by [(11)C]DTBZ binding) is not coregulated with dopamine synthesis. This is in keeping with a role for VMAT2 in other cellular processes (i.e., sequestration and release from the cell of potential toxic products), in addition to its importance for the quantal release of monoamines.
http://www.ncbi.nlm....t_uids=12710012
How does this all tie together?
(1) If the axons and the associated synaptic trees for DA neurons are present in the brain, then there will be vesicles in the presynaptic bulbs that (usually) contain some level of DA. The DA gets into the vesicle by way of a transporter, the vesicular monoamine transporter (VMAT). This is merely some information on the structure of DA neurons and their synaptic projections.
(2) So, if VMAT levels are normal in a brain, then we have very good reason to believe that the synaptic structure is still present in the brain. Whether or not it is functioning correctly is a very different question.
(3) To address whether or not those synaptic trees are functioning correctly, looking at measures of DAT, DA receptors, Tyrosine Hydroxylase are going to be what matters. These markers are markers of how the tree is functioning, and dysregulation of one or more of these will usually be present in a DA-related disease that is not associated with structural degeneration.
I think that my claim at the top has been established: DAT does go down in MA abusers, suggesting impaired functionality; VMAT does not go down in MA abusers, suggesting intact tree structure; VMAT does go down in parkinsons, suggesting that it is a reliable marker of structural damage. What do you think?
Luv2increase, I wouldn't mind showing you at all. Also, I called it pop science because it was in the New York Times. If you would have cited the original paper from the start, then it wouldn't have been accurate for me to say that. But you didn't. Most pop science has references somewhere, but careful reading of those references does not always yeild the same conclusion as the one presented in the pop science presentation of those references. (luv2increase, I have seen you around mind and muscle. I have posted there on various aspects of the DA systems)
Nootropikamil, my primary source for those comments are the lectures given by Professor Anagnostaras in my Drugs & Behavior class at UCSD (Psych 181). I believe you went to UCSD as well, but I am not sure if you have taken this course or even heard of it. From the powerpoint lecture on amphetamines (which I can link to: http://psy.ucsd.edu/...nos/181lec6.ppt), he references this paper - Wilson (1996): http://www.nature.co....861158020.html, or http://www.ncbi.nlm....st_uids=8640565 for the pubmed versionThis quote references the Wilson (1996) that I linked to above, as well as some more recent papers [papers as recent as the one you linked to].However, striatal concentrations of one marker, the vesicular monoamine transporter (VMAT2), considered to be a somewhat more ‘stable’ marker of striatal dopamine nerve terminal integrity (Vander Borght et al., 1995; Wilson and Kish 1996; but see Riddle et al., 2002 and de la Fuente-Fernández et al., 2003), are normal in postmortem brain of MA users (Wilson et al., 1996a) whereas in living brain of self-reported MA users (using PET) VMAT2 levels are, at most, only slightly reduced (personal communication, C. Schuster and C.-E. Johanson, Wayne State University, Detroit MI; K. Frey, University of Michigan, Ann Arbor MI). These data suggest that striatal dopamine nerve terminal number might not be substantially decreased in human MA users.
http://brain.oxfordj.../full/127/2/363
EDIT: This is one of the papers referenced in the above quote, the de la Fuente-Fernández et al. (2003):As for the Thompson et al. (2004) paper you linked to, I have a couple comments on it:Dopa-responsive dystonia (DRD) is a lifelong disorder in which dopamine deficiency is not associated with neuronal loss and therefore it is an ideal human model for investigating the compensatory changes that occur in response to this biochemical abnormality. Using positron emission tomography (PET), we examined the (+/-)-alpha-[(11)C]dihydrotetrabenazine ([(11)C]DTBZ) binding potential of untreated DRD patients and normal controls. Two other PET markers of presynaptic nigrostriatal function, d-threo-[(11)C]methylphenidate ([(11)C]MP) and 6-[(18)F]fluoro-L-dopa ([(18)F]-dopa), and [(11)C]raclopride were also used in the study. We found increased [(11)C]DTBZ binding potential in the striatum of DRD patients. By contrast, no significant changes were detected in either [(11)C]MP binding potential or [(18)F]-dopa uptake rate constant. In addition, we found evidence for increased dopamine turnover in one DRD patient by examining changes in [(11)C]raclopride binding potential in relation to levodopa treatment. We propose that the increase in [(11)C]DTBZ binding likely reflects the dramatic decrease in the intravesicular concentration of dopamine that occurs in DRD; upregulation of vesicular monoamine transporter type 2 (VMAT2) expression may also contribute. Our findings suggest that the striatal expression of VMAT2 (as estimated by [(11)C]DTBZ binding) is not coregulated with dopamine synthesis. This is in keeping with a role for VMAT2 in other cellular processes (i.e., sequestration and release from the cell of potential toxic products), in addition to its importance for the quantal release of monoamines.
http://www.ncbi.nlm....t_uids=12710012
(1) "current Axis I diagnoses other than MA or nicotine dependence were exclusionary for the MA abuser group"; "Axis II disorders were not exclusionary" - Pretty good, I'm glad to see a decent design used on occasion, although I wonder what the prevalence of OCD, Antisocial PD, or other personality disorders (i.e., the Axis II disorders) are for MA abusers, and whether those disorders would show similar MRI results.
(2) "Participants completed self-report drug-use questionnaires [intake questionnaire, drug-use survey, and Addiction Severity Index (McLellan et al., 1992)]. The MA abusers had used the drug (primarily by smoking) for 10.5 years on average, beginning in their mid-twenties. They consumed ~3 gm of MA per week, having used MA on most of the 30 d before entering the study. The groups reported similar alcohol use. Most of the MA abusers but only two of the controls, however, smoked tobacco cigarettes." - There are a few things to note here. First, 10 years is a very long time to be doing MA for and I really wouldn't be surprised if they had cell death after that long because of malnutrition and lack of sleep (things not discussed or accounted for yet in the paper). Second, 3.5 grams is an 1/8 ounce, aka an 8ball. If they were using an 8ball every week there is no way that I know of that they could possibly be getting enough sleep or proper nutrition. (Remember they screened out MA abusers who abused other substances - like benzos or opiates that could help one sleep on that much MA). Finally, they are not abstinent users of MA, as most used up to the day of the study.
The study held one other surprise, Thompson said.
White matter, composed of nerve fibres that connect different areas, was severely inflamed, making the addicts' brains 10 per cent larger than normal.
"This was shocking," he said.
But there was one piece of good news. The white matter was not dead. With abstinence, it might recover.
Posted 08 April 2007 - 08:07 AM
Nootropikamil, my primary source for those comments are the lectures given by Professor Anagnostaras in my Drugs & Behavior class at UCSD (Psych 181). I believe you went to UCSD as well, but I am not sure if you have taken this course or even heard of it. From the powerpoint lecture on amphetamines (which I can link to: http://psy.ucsd.edu/...nos/181lec6.ppt), he references this paper - Wilson (1996): http://www.nature.co....861158020.html, or http://www.ncbi.nlm....st_uids=8640565 for the pubmed version
This quote references the Wilson (1996) that I linked to above, as well as some more recent papers [papers as recent as the one you linked to].However, striatal concentrations of one marker, the vesicular monoamine transporter (VMAT2), considered to be a somewhat more ‘stable’ marker of striatal dopamine nerve terminal integrity (Vander Borght et al., 1995; Wilson and Kish 1996; but see Riddle et al., 2002 and de la Fuente-Fernández et al., 2003), are normal in postmortem brain of MA users (Wilson et al., 1996a) whereas in living brain of self-reported MA users (using PET) VMAT2 levels are, at most, only slightly reduced (personal communication, C. Schuster and C.-E. Johanson, Wayne State University, Detroit MI; K. Frey, University of Michigan, Ann Arbor MI). These data suggest that striatal dopamine nerve terminal number might not be substantially decreased in human MA users.
http://brain.oxfordj.../full/127/2/363
EDIT: This is one of the papers referenced in the above quote, the de la Fuente-Fernández et al. (2003):As for the Thompson et al. (2004) paper you linked to, I have a couple comments on it:Dopa-responsive dystonia (DRD) is a lifelong disorder in which dopamine deficiency is not associated with neuronal loss and therefore it is an ideal human model for investigating the compensatory changes that occur in response to this biochemical abnormality. Using positron emission tomography (PET), we examined the (+/-)-alpha-[(11)C]dihydrotetrabenazine ([(11)C]DTBZ) binding potential of untreated DRD patients and normal controls. Two other PET markers of presynaptic nigrostriatal function, d-threo-[(11)C]methylphenidate ([(11)C]MP) and 6-[(18)F]fluoro-L-dopa ([(18)F]-dopa), and [(11)C]raclopride were also used in the study. We found increased [(11)C]DTBZ binding potential in the striatum of DRD patients. By contrast, no significant changes were detected in either [(11)C]MP binding potential or [(18)F]-dopa uptake rate constant. In addition, we found evidence for increased dopamine turnover in one DRD patient by examining changes in [(11)C]raclopride binding potential in relation to levodopa treatment. We propose that the increase in [(11)C]DTBZ binding likely reflects the dramatic decrease in the intravesicular concentration of dopamine that occurs in DRD; upregulation of vesicular monoamine transporter type 2 (VMAT2) expression may also contribute. Our findings suggest that the striatal expression of VMAT2 (as estimated by [(11)C]DTBZ binding) is not coregulated with dopamine synthesis. This is in keeping with a role for VMAT2 in other cellular processes (i.e., sequestration and release from the cell of potential toxic products), in addition to its importance for the quantal release of monoamines.
http://www.ncbi.nlm....t_uids=12710012
(1) "current Axis I diagnoses other than MA or nicotine dependence were exclusionary for the MA abuser group"; "Axis II disorders were not exclusionary" - Pretty good, I'm glad to see a decent design used on occasion, although I wonder what the prevalence of OCD, Antisocial PD, or other personality disorders (i.e., the Axis II disorders) are for MA abusers, and whether those disorders would show similar MRI results.
Axis I: Clinical Syndromes
This is what we typically think of as the diagnosis (e.g., depression, schizophrenia, social phobia)
Axis II: Developmental Disorders and Personality Disorders
Developmental disorders include autism and mental retardation, disorders which are typically first evident in childhood
Personality disorders are clinical syndromes which have a more long lasting symptoms and encompass the individual's way of interacting with the world. They include Paranoid, Antisocial, and Borderline Personality Disorders.
The current DSM
Categorization
The DSM-IV is a categorical classification system. The categories are prototypes, and a patient with a close approximation to the prototype is said have that disorder. DSM-IV states that “there is no assumption that each category of mental disorder is a completely discrete entity with absolute boundaries...” but isolated, low-grade and noncriterion (unlisted for a given disorder) symptoms are not given importance.[9] Qualifiers are sometimes used, for example mild, moderate or severe forms of a disorder. The DSM-IV also introduced a diagnostic criterion of “clinically significant distress or impairment in social, occupational, or other important areas of functioning", although DSM-IV-TR removed this distress criterion from tic disorders and several of the paraphilias. Each category of disorder has a numeric code taken from the ICD coding system, used for health service (including insurance) adminstrative purposes.
[edit] Multi-axial system
The DSM-IV organizes each psychiatric diagnosis into five levels (axes) relating to different aspects of disorder or disability:
Axis I: clinical disorders, including major mental disorders, as well as developmental and learning disorders
Axis II: underlying pervasive or personality conditions, as well as mental retardation
Axis III: medical conditions which may be relevant to the understanding and treatment of the mental disorder
Axis IV: psychosocial and environmental factors contributing to the disorder
Axis V: Global Assessment of Functioning (on a scale from 100 to 0 — GAF score)
Common Axis I disorders include depression, anxiety disorders, bipolar disorder, ADHD, and schizophrenia.
Common Axis II disorders include borderline personality disorder, schizotypal personality disorder, antisocial personality disorder, narcissistic personality disorder, and mild mental retardation.
This is an MRI of the human brain done here at UCLA and this shows the judgment center of the brain in the prefrontal cortex. This is the brain of a meth user who's about five days sober and this blue area represents a reduction in normal activity, a reduction in blood flow. In essence, this part of the brain is shut off and for meth users who are in early recovery, they really don't have the ability to make good decisions.
You have this sort of worst-case scenario. You have a brain that is not producing reward, you're having a lot of craving because you want to feel better, and you have the part of the brain that controls judgment not working, and so individuals do stupid things that end up with them relapsing and going back to using. It's a wonder any meth users ever get better, but in fact they do.
Edited by nootropikamil, 08 April 2007 - 08:43 AM.
Posted 17 April 2007 - 03:24 AM
(3) "To our knowledge, this study is the first to demonstrate systematic brain structural deficits in MA abusers. It has some limitations, however. It is not yet clear how these deficits emerge over time, whether they are progressive, and to what extent therapy or abstinence may reverse them. Another potential limitation relates to matching of the two groups. Although the groups were well matched on most categories, most of the MA abusers and only two of the control subjects were tobacco smokers. A recent study of brain structure found that smokers had smaller gray-matter volumes and lower gray-matter densities than nonsmokers in the prefrontal cortex (primarily in the bilateral dorsolateral prefrontal cortex but also in the left ventrolateral prefrontal cortex), along with smaller volumes in the left dorsal anterior cingulate gyrus and lower gray-matter densities in the right cerebellum (Brody et al., 2004). The effect related to smoking in the cingulate gyrus (dorsal, mid-cingulate area) was much more restricted than the current finding, which extended through the entire cingulate gyrus. Furthermore, no evidence of hippocampal abnormality was observed." - Good, they acknowledged some important limitations of their study. Although I do think the worry about smoking is over emphasized, it is interesting that similar deficiencies were found in smokers.
Reuters Health: News Source
Smoking lowers Parkinson's disease risk
Tue Mar 20, 2007 2:03PM EDT
By Megan Rauscher
NEW YORK (Reuters Health) - A new study adds to the previously reported evidence that cigarette smoking protects against Parkinson's disease. Specifically, the new research shows a temporal relationship between smoking and reduced risk of Parkinson's disease. That is, the protective effect wanes after smokers quit.
"It is not our intent to promote smoking as a protective measure against Parkinson's disease," Evan L. Thacker from Harvard School of Public Health emphasized in comments to Reuters Health. "Obviously smoking has a multitude of negative consequences. Rather, we did this study to try to encourage other scientists...to consider the possibility that neuroprotective chemicals may be present in tobacco leaves."
As reported in the March 6th issue of Neurology, Thacker and colleagues analyzed data, including detailed lifetime smoking histories, from 79,977 women and 63,348 men participating in the Cancer Prevention Study II Nutrition Cohort. During about 9 years of follow-up, 413 subjects developed definite or probable Parkinson's disease.
Compared to people who had never smoked and were considered to have "normal" Parkinson's disease risk, former smokers had a 22-percent lower risk of Parkinson's disease and current smokers had a 73-percent lower risk.
"The results were similar for men and women, and were also similar to the results of studies by many other researchers looking at the same topic," Thacker noted.
In former smokers, more years of smoking, fewer years since quitting, more cigarettes per day, and a higher total amount of lifetime smoking were all related to a lower Parkinson's disease risk. The researchers also found that the duration of smoking and the time since quitting influenced risk more than the average daily amount of smoking.
"A 30 percent to 60 percent decreased risk of Parkinson's disease was apparent for smoking as early as 15 to 24 years before symptom onset, but not for smoking 25 or more years before onset," the investigators report.
"The results of our study," Thacker said, "can probably be explained by something in cigarettes -- most likely in the tobacco itself -- actually protecting people against getting Parkinson's disease. That would be the simplest explanation that makes the most sense."
Studies to determine if, in fact, there are neuroprotective compounds in tobacco are warranted, the researchers say. "The observation that smokeless tobacco users also have a lower risk of Parkinson's disease suggests that the most likely candidates are not compounds generated by combustion, but rather constituents of the tobacco leaves."
SOURCE: Neurology, March 6,, 2007.
© Reuters 2006. All rights reserved. Republication or redistribution of Reuters content, including by caching, framing or similar means, is expressly prohibited without the prior written consent of Reuters. Reuters and the Reuters sphere logo are registered trademarks and trademarks of the Reuters group of companies around the world.
Reuters journalists are subject to the Reuters Editorial Handbook which requires fair presentation and disclosure of relevant interests.
Neuropharmacology. 2004;47 Suppl 1:92-100.
The methamphetamine experience: a NIDA partnership.
Hanson GR, Rau KS, Fleckenstein AE.
Department of Pharmacology and Toxicology, University of Utah, 30 South 2000 East, Skaggs Hall, Room 112, Salt Lake City, UT 84112, USA. glen.hanson@hsc.utah.edu
The neurotoxic properties of the amphetamines such as methamphetamine (METH) were originally described about the time of the National Institute on Drug Abuse's organization, in the early 1970s. It required more than 20 years to confirm these neurotoxic properties in humans. Much like Parkinson's disease, multiple high-dose administration of METH somewhat selectively damages the nigrostriatal dopamine (DA) projection of the brain. This effect appears to be related to the intracellular accumulation of cytosolic DA and its ability to oxidize into reactive oxygen species. Both the dopamine plasmalemmal transporter and the vesicular monoamine transporter-2 seem to play critical roles in this neurotoxicity. METH and related analogs such as methylenedioxymethamphetamine (MDMA) can also damage selective CNS serotonin neurons. The mechanism of the serotonergic neurotoxicity is not as well characterized, but also appears to be related to the formation of reactive oxygen species and monoamine transporters. Studies examining the pharmacological and neurotoxicological properties of the amphetamines have helped to elucidate some critical features of monoamine regulations as well as helped to improve our understanding of the processes associated with degenerative disorders such as Parkinson's disease.
Publication Types:
Review
PMID: 15464128 [PubMed - indexed for MEDLINE]
Over all, it is a good study. However, I wouldn't be so quick to say that the decrease in gray-matter volume is attributable to MA in itself, but rather very long term MA addiction at very high doses along with the coincident lack of hygiene, of proper nutrition, and of proper sleep.
Edited by nootropikamil, 17 April 2007 - 04:09 AM.
Posted 19 April 2007 - 08:42 AM
You are right that my first post was poorly worded and prone to misinterpretation, and that it was out of line as well.
Since I, in fact, did cite the references previously, I will now quote myself and spell it out for you.I'm not sure, but I didn't see a shred of evidence supporting any your points in your first post in this topic; meanwhile you dismiss other fine journalists' work as "pop science."
Here is my claim in the first post:Using a measure of DAT levels is not a good indicator of synaptic damage or degeneration. DAT levels are down regulated in the same way that postsynaptic DA receptors are. A measure of VMAT levels is more indicative of whether there has been actual degeneration. Studies have been done on methamphetamine users and they do not show significant losses in VMAT. So while there is down regulation in the functionality of the neurons, there isn't much evidence to show actual synaptic degeneration or neuronal death. This is especially true at the doses that methamphetamine users take. The doses that are used in rats to cause neurotoxicity are much higher than the actual street doses (unlike, for example, MDMA, where the street dose is neurotoxic).
In my second post I wrote:
Now, to quote from the Wilson (1996) study:That is, the found that DAT went down in MA abusers, but VMAT (which is known to be reduced in parkisonian patients, who have synaptic degeneration) was not reduced.We found reduced levels of three dopamine nerve terminal markers (dopamine, tyrosine hydroxylase and the dopamine transporter) in post-mortem striatum (nucleus accumbens, caudate, putamen) of chronic methamphetamine users. However, levels of DOPA decarboxylase and the vesicular monoamine transporter, known to be reduced in Parkinson's disease were normal. This suggests that chronic exposure to methamphetamine does not cause permanent degeneration of striatal dopamine nerve terminals at the doses used by the young subjects in our study.
http://www.nature.co....861158020.htmlThis reiterates what was found by Wilson (1996), and adds to it, showing results from living MA abusers as well.However, striatal concentrations of one marker, the vesicular monoamine transporter (VMAT2), considered to be a somewhat more ‘stable’ marker of striatal dopamine nerve terminal integrity (Vander Borght et al., 1995; Wilson and Kish 1996; but see Riddle et al., 2002 and de la Fuente-Fernández et al., 2003), are normal in postmortem brain of MA users (Wilson et al., 1996a) whereas in living brain of self-reported MA users (using PET) VMAT2 levels are, at most, only slightly reduced (personal communication, C. Schuster and C.-E. Johanson, Wayne State University, Detroit MI; K. Frey, University of Michigan, Ann Arbor MI). These data suggest that striatal dopamine nerve terminal number might not be substantially decreased in human MA users.
http://brain.oxfordj.../full/127/2/363The important part here is that regulation of DA synthesis does not regulate VMAT, showing the independence of the two processes.Dopa-responsive dystonia (DRD) is a lifelong disorder in which dopamine deficiency is not associated with neuronal loss and therefore it is an ideal human model for investigating the compensatory changes that occur in response to this biochemical abnormality. Using positron emission tomography (PET), we examined the (+/-)-alpha-[(11)C]dihydrotetrabenazine ([(11)C]DTBZ) binding potential of untreated DRD patients and normal controls. Two other PET markers of presynaptic nigrostriatal function, d-threo-[(11)C]methylphenidate ([(11)C]MP) and 6-[(18)F]fluoro-L-dopa ([(18)F]-dopa), and [(11)C]raclopride were also used in the study. We found increased [(11)C]DTBZ binding potential in the striatum of DRD patients. By contrast, no significant changes were detected in either [(11)C]MP binding potential or [(18)F]-dopa uptake rate constant. In addition, we found evidence for increased dopamine turnover in one DRD patient by examining changes in [(11)C]raclopride binding potential in relation to levodopa treatment. We propose that the increase in [(11)C]DTBZ binding likely reflects the dramatic decrease in the intravesicular concentration of dopamine that occurs in DRD; upregulation of vesicular monoamine transporter type 2 (VMAT2) expression may also contribute. Our findings suggest that the striatal expression of VMAT2 (as estimated by [(11)C]DTBZ binding) is not coregulated with dopamine synthesis. This is in keeping with a role for VMAT2 in other cellular processes (i.e., sequestration and release from the cell of potential toxic products), in addition to its importance for the quantal release of monoamines.
http://www.ncbi.nlm....t_uids=12710012
How does this all tie together?
(1) If the axons and the associated synaptic trees for DA neurons are present in the brain, then there will be vesicles in the presynaptic bulbs that (usually) contain some level of DA. The DA gets into the vesicle by way of a transporter, the vesicular monoamine transporter (VMAT). This is merely some information on the structure of DA neurons and their synaptic projections.
(2) So, if VMAT levels are normal in a brain, then we have very good reason to believe that the synaptic structure is still present in the brain. Whether or not it is functioning correctly is a very different question.
(3) To address whether or not those synaptic trees are functioning correctly, looking at measures of DAT, DA receptors, Tyrosine Hydroxylase are going to be what matters. These markers are markers of how the tree is functioning, and dysregulation of one or more of these will usually be present in a DA-related disease that is not associated with structural degeneration.
I think that my claim at the top has been established: DAT does go down in MA abusers, suggesting impaired functionality; VMAT does not go down in MA abusers, suggesting intact tree structure; VMAT does go down in parkinsons, suggesting that it is a reliable marker of structural damage.
What do you think?
Posted 26 April 2007 - 07:59 AM
News Source: Newsday.com
Study: Meth Use in Rural Areas Riskier
By TIMBERLY ROSS
Associated Press Writer
April 24, 2007, 9:10 PM EDT
OMAHA, Neb. -- Methamphetamine abusers in rural areas have more medical and psychiatric problems that may inhibit recovery than their urban counterparts, according to a new study that compares the two groups.
Experts say the findings are unsettling because rural addicts have limited access to treatment facilities and health professionals.
"Rural methamphetamine is worse in a lot of respects," said lead researcher Dr. Kathleen Grant, who works at the Omaha VA Medical Center and the University of Nebraska Medical Center.
Meth is an addictive stimulant that can be prepared or "cooked" in makeshift labs with over-the-counter cold tablets, common household chemicals and fertilizers.
According to the 2004 National Survey on Drug Use and Health, about 11.7 million Americans ages 12 and older said they've tried methamphetamine and 1.4 million said they'd used it in the past month.
The study, funded by the state, compared addicts from a 20,000-square-mile region who sought help at the nearest treatment facility in Grand Island with those living near and seeking help in state's two largest cities, Omaha and Lincoln. In all, 172 meth abusers were interviewed between July 2004 and July 2005.
The study showed that rural addicts began using meth at a younger age, were more likely to use the drug intravenously and were more likely to also be dependent on alcohol or cigarettes. They also exhibited more signs of psychosis than urban addicts -- 45 percent vs. 29 percent, according to the study.
Grant said the findings, released in the March/April edition of The American Journal on Addictions, suggest rural addicts are at higher risk for psychiatric and medical problems such as infectious diseases and lung and liver cancer.
That's troubling, she said, because addicts living in rural areas have less access to care -- because of distance and transportation issues -- than those living in cities.
"These people continue to slide into addiction and are not able to get the treatment they need," said Dr. Jennifer Sharpe Potter, an opiate specialist at Harvard-affiliated McLean Hospital in Belmont, Mass.
She said meth addiction is difficult to treat because there are few treatment options available, and often the options that work best are not available in rural areas. That points to what she calls a long-standing problem that reaches beyond drug treatment: the availability of health care services in rural areas.
Recovering meth addict Barry Schmidt, 49, said he had to move from Fort Dodge, Iowa, to Omaha in order to get the help he needed to overcome a lifetime of drug and alcohol abuse. He left his wife and gave up seeing his father, who lives in a nursing home there.
"I changed my playground, playmates and playthings," he said.
It was hard, but something he said was necessary to get over his addictions.
Schmidt said he's been in treatment 19 times over the past 30 years, the first time when he was 19. His environment and a lack of recovery support were obstacles to staying clean, he said.
But things have been different in Omaha. Schmidt said he's graduated from the VA hospital's treatment program and attends six to seven recovery meetings a week.
He credits those meetings and the people he meets there with his success so far.
"I know that if I called any one of them at any given time and said I'm thinking of using and I'm in a bad place, they'd be there for me."
___
On the Web:
University of Nebraska Medical Center:
Copyright 2007 Newsday Inc.
Posted 02 May 2007 - 06:06 PM
Posted 02 July 2007 - 01:59 AM
You are right that my first post was poorly worded and prone to misinterpretation, and that it was out of line as well.
Since I, in fact, did cite the references previously, I will now quote myself and spell it out for you.I'm not sure, but I didn't see a shred of evidence supporting any your points in your first post in this topic; meanwhile you dismiss other fine journalists' work as "pop science."
Here is my claim in the first post:Using a measure of DAT levels is not a good indicator of synaptic damage or degeneration. DAT levels are down regulated in the same way that postsynaptic DA receptors are. A measure of VMAT levels is more indicative of whether there has been actual degeneration. Studies have been done on methamphetamine users and they do not show significant losses in VMAT. So while there is down regulation in the functionality of the neurons, there isn't much evidence to show actual synaptic degeneration or neuronal death. This is especially true at the doses that methamphetamine users take. The doses that are used in rats to cause neurotoxicity are much higher than the actual street doses (unlike, for example, MDMA, where the street dose is neurotoxic).
In my second post I wrote:
Now, to quote from the Wilson (1996) study:That is, the found that DAT went down in MA abusers, but VMAT (which is known to be reduced in parkisonian patients, who have synaptic degeneration) was not reduced.We found reduced levels of three dopamine nerve terminal markers (dopamine, tyrosine hydroxylase and the dopamine transporter) in post-mortem striatum (nucleus accumbens, caudate, putamen) of chronic methamphetamine users. However, levels of DOPA decarboxylase and the vesicular monoamine transporter, known to be reduced in Parkinson's disease were normal. This suggests that chronic exposure to methamphetamine does not cause permanent degeneration of striatal dopamine nerve terminals at the doses used by the young subjects in our study.
http://www.nature.co....861158020.htmlThis reiterates what was found by Wilson (1996), and adds to it, showing results from living MA abusers as well.However, striatal concentrations of one marker, the vesicular monoamine transporter (VMAT2), considered to be a somewhat more ‘stable’ marker of striatal dopamine nerve terminal integrity (Vander Borght et al., 1995; Wilson and Kish 1996; but see Riddle et al., 2002 and de la Fuente-Fernández et al., 2003), are normal in postmortem brain of MA users (Wilson et al., 1996a) whereas in living brain of self-reported MA users (using PET) VMAT2 levels are, at most, only slightly reduced (personal communication, C. Schuster and C.-E. Johanson, Wayne State University, Detroit MI; K. Frey, University of Michigan, Ann Arbor MI). These data suggest that striatal dopamine nerve terminal number might not be substantially decreased in human MA users.
http://brain.oxfordj.../full/127/2/363The important part here is that regulation of DA synthesis does not regulate VMAT, showing the independence of the two processes.Dopa-responsive dystonia (DRD) is a lifelong disorder in which dopamine deficiency is not associated with neuronal loss and therefore it is an ideal human model for investigating the compensatory changes that occur in response to this biochemical abnormality. Using positron emission tomography (PET), we examined the (+/-)-alpha-[(11)C]dihydrotetrabenazine ([(11)C]DTBZ) binding potential of untreated DRD patients and normal controls. Two other PET markers of presynaptic nigrostriatal function, d-threo-[(11)C]methylphenidate ([(11)C]MP) and 6-[(18)F]fluoro-L-dopa ([(18)F]-dopa), and [(11)C]raclopride were also used in the study. We found increased [(11)C]DTBZ binding potential in the striatum of DRD patients. By contrast, no significant changes were detected in either [(11)C]MP binding potential or [(18)F]-dopa uptake rate constant. In addition, we found evidence for increased dopamine turnover in one DRD patient by examining changes in [(11)C]raclopride binding potential in relation to levodopa treatment. We propose that the increase in [(11)C]DTBZ binding likely reflects the dramatic decrease in the intravesicular concentration of dopamine that occurs in DRD; upregulation of vesicular monoamine transporter type 2 (VMAT2) expression may also contribute. Our findings suggest that the striatal expression of VMAT2 (as estimated by [(11)C]DTBZ binding) is not coregulated with dopamine synthesis. This is in keeping with a role for VMAT2 in other cellular processes (i.e., sequestration and release from the cell of potential toxic products), in addition to its importance for the quantal release of monoamines.
http://www.ncbi.nlm....t_uids=12710012
How does this all tie together?
(1) If the axons and the associated synaptic trees for DA neurons are present in the brain, then there will be vesicles in the presynaptic bulbs that (usually) contain some level of DA. The DA gets into the vesicle by way of a transporter, the vesicular monoamine transporter (VMAT). This is merely some information on the structure of DA neurons and their synaptic projections.
(2) So, if VMAT levels are normal in a brain, then we have very good reason to believe that the synaptic structure is still present in the brain. Whether or not it is functioning correctly is a very different question.
(3) To address whether or not those synaptic trees are functioning correctly, looking at measures of DAT, DA receptors, Tyrosine Hydroxylase are going to be what matters. These markers are markers of how the tree is functioning, and dysregulation of one or more of these will usually be present in a DA-related disease that is not associated with structural degeneration.
I think that my claim at the top has been established: DAT does go down in MA abusers, suggesting impaired functionality; VMAT does not go down in MA abusers, suggesting intact tree structure; VMAT does go down in parkinsons, suggesting that it is a reliable marker of structural damage.
What do you think?
I think you've lost me now... I've never heard of VMAT before... please give me a little while to catch up here...
(3) "To our knowledge, this study is the first to demonstrate systematic brain structural deficits in MA abusers. It has some limitations, however. It is not yet clear how these deficits emerge over time, whether they are progressive, and to what extent therapy or abstinence may reverse them. Another potential limitation relates to matching of the two groups. Although the groups were well matched on most categories, most of the MA abusers and only two of the control subjects were tobacco smokers. A recent study of brain structure found that smokers had smaller gray-matter volumes and lower gray-matter densities than nonsmokers in the prefrontal cortex (primarily in the bilateral dorsolateral prefrontal cortex but also in the left ventrolateral prefrontal cortex), along with smaller volumes in the left dorsal anterior cingulate gyrus and lower gray-matter densities in the right cerebellum (Brody et al., 2004). The effect related to smoking in the cingulate gyrus (dorsal, mid-cingulate area) was much more restricted than the current finding, which extended through the entire cingulate gyrus. Furthermore, no evidence of hippocampal abnormality was observed." - Good, they acknowledged some important limitations of their study. Although I do think the worry about smoking is over emphasized, it is interesting that similar deficiencies were found in smokers.
Mr. Kite:
A recent report published in the media seems to suggest that cigarette smoking protects against Parkinson's disease:Reuters Health: News Source
Smoking lowers Parkinson's disease risk
Tue Mar 20, 2007 2:03PM EDT
By Megan Rauscher
NEW YORK (Reuters Health) - A new study adds to the previously reported evidence that cigarette smoking protects against Parkinson's disease. Specifically, the new research shows a temporal relationship between smoking and reduced risk of Parkinson's disease. That is, the protective effect wanes after smokers quit.
"It is not our intent to promote smoking as a protective measure against Parkinson's disease," Evan L. Thacker from Harvard School of Public Health emphasized in comments to Reuters Health. "Obviously smoking has a multitude of negative consequences. Rather, we did this study to try to encourage other scientists...to consider the possibility that neuroprotective chemicals may be present in tobacco leaves."
As reported in the March 6th issue of Neurology, Thacker and colleagues analyzed data, including detailed lifetime smoking histories, from 79,977 women and 63,348 men participating in the Cancer Prevention Study II Nutrition Cohort. During about 9 years of follow-up, 413 subjects developed definite or probable Parkinson's disease.
Compared to people who had never smoked and were considered to have "normal" Parkinson's disease risk, former smokers had a 22-percent lower risk of Parkinson's disease and current smokers had a 73-percent lower risk.
"The results were similar for men and women, and were also similar to the results of studies by many other researchers looking at the same topic," Thacker noted.
In former smokers, more years of smoking, fewer years since quitting, more cigarettes per day, and a higher total amount of lifetime smoking were all related to a lower Parkinson's disease risk. The researchers also found that the duration of smoking and the time since quitting influenced risk more than the average daily amount of smoking.
"A 30 percent to 60 percent decreased risk of Parkinson's disease was apparent for smoking as early as 15 to 24 years before symptom onset, but not for smoking 25 or more years before onset," the investigators report.
"The results of our study," Thacker said, "can probably be explained by something in cigarettes -- most likely in the tobacco itself -- actually protecting people against getting Parkinson's disease. That would be the simplest explanation that makes the most sense."
Studies to determine if, in fact, there are neuroprotective compounds in tobacco are warranted, the researchers say. "The observation that smokeless tobacco users also have a lower risk of Parkinson's disease suggests that the most likely candidates are not compounds generated by combustion, but rather constituents of the tobacco leaves."
SOURCE: Neurology, March 6,, 2007.
© Reuters 2006. All rights reserved. Republication or redistribution of Reuters content, including by caching, framing or similar means, is expressly prohibited without the prior written consent of Reuters. Reuters and the Reuters sphere logo are registered trademarks and trademarks of the Reuters group of companies around the world.
Reuters journalists are subject to the Reuters Editorial Handbook which requires fair presentation and disclosure of relevant interests.
Click here for further discussion of that matter.
How exactly is this issue related to your comments regarding how smoking might affect the results of MRIs measuring grey matter volume of meth abusers compared with a set of matched controls? Isn't it true that similarly to meth abuse, Parkinson's disease itself is also related to decline of the dopaminergic system? Might that imply a neuroprotective role of nicotine (or smoking?) in this context?
Wouldn't you expect that, based on this recent report, that the meth abusers who smoked tobacco to have a little bit more dopaminergic based grey matter volumes than the non smokers -- and if so, could that possibly affect the difference of grey matter in the MRIs detected between the control group smokers and non smokers and the meth abusing smokers and non smokers if not selected for equally prior to randomization?
Again, I'll cite the following abstract:Neuropharmacology. 2004;47 Suppl 1:92-100.
The methamphetamine experience: a NIDA partnership.
Hanson GR, Rau KS, Fleckenstein AE.
Department of Pharmacology and Toxicology, University of Utah, 30 South 2000 East, Skaggs Hall, Room 112, Salt Lake City, UT 84112, USA. glen.hanson@hsc.utah.edu
The neurotoxic properties of the amphetamines such as methamphetamine (METH) were originally described about the time of the National Institute on Drug Abuse's organization, in the early 1970s. It required more than 20 years to confirm these neurotoxic properties in humans. Much like Parkinson's disease, multiple high-dose administration of METH somewhat selectively damages the nigrostriatal dopamine (DA) projection of the brain. This effect appears to be related to the intracellular accumulation of cytosolic DA and its ability to oxidize into reactive oxygen species. Both the dopamine plasmalemmal transporter and the vesicular monoamine transporter-2 seem to play critical roles in this neurotoxicity. METH and related analogs such as methylenedioxymethamphetamine (MDMA) can also damage selective CNS serotonin neurons. The mechanism of the serotonergic neurotoxicity is not as well characterized, but also appears to be related to the formation of reactive oxygen species and monoamine transporters. Studies examining the pharmacological and neurotoxicological properties of the amphetamines have helped to elucidate some critical features of monoamine regulations as well as helped to improve our understanding of the processes associated with degenerative disorders such as Parkinson's disease.
Publication Types:
Review
PMID: 15464128 [PubMed - indexed for MEDLINE]Over all, it is a good study. However, I wouldn't be so quick to say that the decrease in gray-matter volume is attributable to MA in itself, but rather very long term MA addiction at very high doses along with the coincident lack of hygiene, of proper nutrition, and of proper sleep.
Now, onto your second point -- I already sort of tried to address this point a few posts above. But the decline in grey matter is at least partially attributed to neurotoxicity attributed to MA use, as this has been proven in human postmortem studies and also through a couple of decades of extensive animal research.
The fact that meth can keep folks awake for days at a time gives you a pretty good idea of how dangerous of a drug we are discussing here. No other drug I know of seems to be able to do that.
Yes, perhaps lack of sleep, poor hygiene, in combination with malnutrition may contribute to decline in grey matter, but no one can deny that methamphetamine is playing the "starring role" in this brain destruction.
More on the rest of your points later....until then...
Take care.
Posted 15 July 2007 - 04:36 AM


American Meth is a cross-country journey that focuses on several facets of the methamphetamine epidemic. From the oil fields of Wyoming and New Mexico to the homeless in Portland and the teens of Montana, filmmaker Justin Hunt spins a blue-collar tale of tragedy and triumph.
Actor Val Kilmer lends his voicing talents as your narrator while exploring both the damage being done and community efforts to take back America.
The movie culminates with the introduction of James and Holly, a pair of meth addicts, and the parents of four children, who let Justin into their lives.
American Meth does two things: It informs of the devastation that this drug is imposing on our country, and it encourages Americans that it is possible to reclaim our friends, our neighbors, our families, one person at a time.
Copyright © 2007 American Meth. All Rights Reserved.
Posted 15 July 2007 - 03:20 PM
Posted 15 July 2007 - 05:56 PM
0 members, 1 guests, 0 anonymous users